Perimenopause supplements can be a powerful tool for women navigating the hormonal rollercoaster that begins in the years leading up to menopause. During this transitional phase—often beginning in the late 30s or early 40s—estrogen and progesterone levels fluctuate unpredictably, triggering a wide range of symptoms: hot flashes, anxiety, brain fog, fatigue, irregular cycles, and more.

While food, sleep, movement, and stress management form the foundation of hormonal health, supplements can offer targeted support when nutrient needs rise or imbalances become difficult to manage through lifestyle alone. Nutrient depletion is common in perimenopause due to stress, inflammation, and the demands of hormone metabolism. Additionally, some women may face absorption issues or genetic variants like MTHFR that affect how their bodies use nutrients such as folate or B12.
This article explores the most effective, evidence-based supplements that can ease perimenopausal symptoms and promote hormonal balance. We’ll also look at targeted support for symptoms like hot flashes, mood swings, low libido, and brain fog, as well as tips on selecting high-quality products and when to consult with a healthcare provider.
Why Supplements Matter in Perimenopause
As estrogen and progesterone levels begin to rise and fall unpredictably during perimenopause, a woman’s nutritional requirements often shift in response. These hormonal changes can place additional stress on systems like the adrenal glands, thyroid, and liver—organs that require a steady supply of key micronutrients to function properly. Unfortunately, this is also a time when many women experience nutrient depletion due to stress, irregular eating habits, poor sleep, digestive issues, or age-related absorption challenges.
Increased levels of inflammation and oxidative stress during perimenopause further accelerate nutrient loss, especially of antioxidants like vitamins C and E, as well as minerals like magnesium and zinc. The body may also struggle to properly detoxify and eliminate excess hormones, leading to symptoms of estrogen dominance such as bloating, heavy periods, and mood swings. This is where targeted supplementation can make a real difference—supporting hormone metabolism, reducing inflammation, and helping the body cope with stress more effectively.
Additionally, perimenopause can impact gut health, which in turn affects hormone clearance. The estrobolome—a collection of gut bacteria involved in estrogen metabolism—plays a crucial role in regulating circulating hormone levels. If the gut is inflamed or imbalanced (a state called dysbiosis), it may reabsorb rather than eliminate excess estrogen, worsening hormonal symptoms.
Supplements are not a shortcut, but they can be powerful allies when used alongside healthy habits. By providing your body with the right building blocks—whether through magnesium to support sleep, B vitamins to boost energy and mood, or omega-3s to reduce inflammation—you can navigate perimenopause with greater ease, resilience, and clarity.
Core Supplements for Perimenopausal Support
The hormonal shifts of perimenopause place new demands on the body—nutritionally, neurologically, and emotionally. While food should be the foundation, certain perimenopause supplements can help fill in critical gaps, ease transition-related symptoms, and support hormone metabolism.
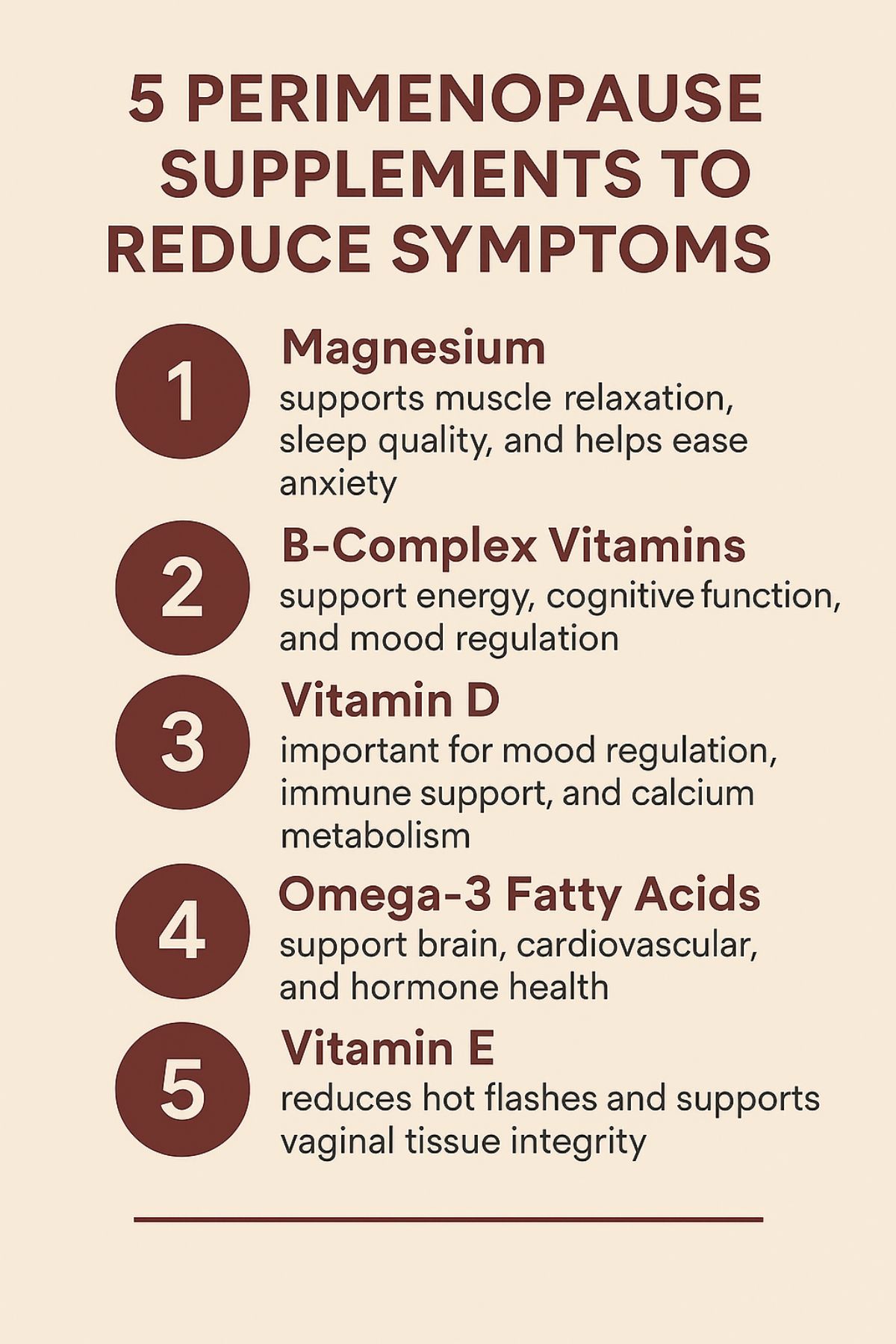
1. Magnesium
Often referred to as nature’s calming mineral, magnesium plays a vital role in over 300 enzymatic processes, including estrogen detoxification, cortisol regulation, and GABA (gamma-aminobutyric acid) production. It supports muscle relaxation, sleep quality, and helps ease anxiety—making it especially beneficial for perimenopausal women struggling with insomnia or mood shifts.
Best forms: Magnesium glycinate (for calm and sleep), magnesium citrate (for constipation).
2. B-Complex Vitamins (Especially B6, B9, and B12)
The B vitamins support energy, cognitive function, mood regulation, and hormone detoxification.
- Vitamin B6 supports serotonin and dopamine production, easing irritability and low mood associated with PMS or PMDD.
- Folate (B9) is crucial for methylation—a process essential for hormone clearance and mood regulation. Women with MTHFR variants should choose methylfolate over folic acid for better absorption
- Vitamin B12, particularly in its methylated form, supports red blood cell production and neurological function. Deficiencies are common in women over 40, especially if they use acid-blocking medications or follow plant-based diets.
These vitamins are especially important during times of chronic stress, as depletion is accelerated when cortisol levels rise.
3. Vitamin D
More than just a vitamin, vitamin D acts like a hormone in the body. It plays a central role in mood regulation, immune support, and calcium metabolism, which is vital for preventing bone loss during midlife. Vitamin D also influences ovarian function and may help regulate menstrual cycles and support fertility.
4. Omega-3 Fatty Acids (EPA and DHA)
EPA and DHA are anti-inflammatory fatty acids found in fish oil that support brain, cardiovascular, and hormone health.
- EPA can help with mood regulation and hot flash reduction.
- DHA is essential for cognitive clarity and nervous system support—both common concerns in perimenopause.
Omega-3s also support healthy cell membranes, which are required for hormone receptor sensitivity.
Plant-based omega-3s (like flaxseed oil) offer ALA, but this form must be converted to EPA/DHA in the body—a process that is inefficient in many adults.
5. Vitamin E
This fat-soluble antioxidant has been shown to reduce hot flashes and support vaginal tissue integrity. It plays a role in reproductive hormone regulation and cellular protection. For optimal absorption, vitamin E should be taken alongside dietary fats.
6. Adaptogens (Ashwagandha, Rhodiola, Maca)
Adaptogens are plant compounds that modulate the body’s stress response, particularly through the hypothalamic-pituitary-adrenal (HPA) axis.
- Ashwagandha helps regulate cortisol, reduce anxiety, and improve sleep.
- Rhodiola has been shown to reduce mental fatigue and improve cognitive resilience under stress.
- Maca root (especially gelatinized forms) supports libido, energy, and hormonal regularity by modulating the HPA-ovarian axis.
These six core supplements—magnesium, B vitamins, vitamin D, omega-3s, vitamin E, and adaptogens—form the backbone of perimenopausal support. Each addresses multiple systems affected by hormonal shifts: brain, adrenal, immune, reproductive, and detoxification. Together, they offer foundational resilience during this phase of profound physiological change.
Targeted Supplements for Specific Perimenopausal Symptoms
While foundational perimenopause supplements like magnesium, B vitamins, and omega-3s offer broad benefits, some symptoms may need more targeted support. The following supplements have been highlighted in both research and clinical education materials for their potential to ease specific perimenopausal complaints.

Hot Flashes & Night Sweats
- Vitamin E has been shown to reduce the severity and frequency of hot flashes, possibly through its antioxidant effects and estrogen receptor support
- Sage extract contains compounds that may reduce thermoregulatory symptoms.
- Black Cohosh is widely used for vasomotor symptoms, though responses are individual.
- Melatonin may improve sleep quality and reduce nighttime hot flashes by modulating circadian rhythms
Mood Swings, Anxiety & Sleep Disturbances
- Magnesium glycinate supports relaxation and better sleep
- Vitamin B6 plays a critical role in neurotransmitter production (serotonin, dopamine, GABA) and can reduce PMS and mood instability
- L-theanine is widely supported in clinical practice for promoting alpha brain waves and calm focus.
- GABA and melatonin can help improve sleep latency and nighttime waking, especially during hormonal fluctuations.
Low Libido & Vaginal Dryness
- Maca root is a libido enhancer that supports the HPA axis and ovarian hormone production
- Omega-3s support blood flow and reduce inflammation, contributing to vaginal tissue health
- Vitamin D aids hormonal signaling and libido regulation
- DHEA may support vaginal tissue and libido, though it requires medical supervision
Brain Fog, Memory & Focus
- Vitamin B12 (preferably as methylcobalamin) supports neurological health and is often depleted in women with low energy or absorption issues
- DHA, a brain-essential omega-3, supports cognition during perimenopause.
- Rhodiola is known to reduce mental fatigue and enhance stress tolerance
- Phosphatidylserine is widely recommended to support memory and cognitive resilience.
Supplements to Be Cautious With
While many perimenopause supplements offer meaningful support, others may carry risks—especially if used without guidance or in excessive doses. Some supplements interact with medications, may not be appropriate for hormone-sensitive conditions, or may worsen symptoms when taken incorrectly. This section outlines key categories of supplements where caution is advised, based on your educational content and broader clinical considerations.
1. DHEA and Bioidentical Hormones
DHEA (dehydroepiandrosterone) is a precursor to estrogen and testosterone and may support libido, vaginal tissue, and energy—but it behaves like a hormone and should not be self-prescribed.
- Work with a licensed healthcare professional to see if this is something that will help you reduce your symptoms
- Improper use can lead to acne, irritability, mood changes, or unwanted hormone shifts.
2. Melatonin (High Doses)
Low-dose melatonin (0.3–1 mg) can help reset circadian rhythms, especially in women with sleep disturbances. However:
- Higher doses (>3 mg) may disrupt sleep architecture, suppress natural melatonin production, and lead to morning grogginess.
- It may also interact with medications, including antidepressants and blood pressure drugs.
If used, start low and titrate only under guidance.
3. Fat-Soluble Vitamins (A, D, E, K)
These vitamins are stored in the body’s fat tissue and can accumulate to toxic levels if over-supplemented:
- Vitamin A: Excessive intake (especially retinol form) is linked to liver toxicity and birth defects.
- Vitamin D: Long-term high doses without monitoring can lead to calcium imbalance and kidney issues.
- Vitamin E: In high doses, may increase bleeding risk or interfere with medications like statins or anticoagulants.
4. Aloe Vera (Whole Leaf)
While inner leaf aloe vera can be beneficial for gut repair, whole-leaf aloe contains aloin, a latex compound with a laxative effect that may irritate the gut and lead to electrolyte imbalance or dependency.
How to Choose High-Quality Supplements
When it comes to perimenopause supplements, quality matters as much as the ingredient itself. Not all supplements are created equal—and poor-quality products may contain contaminants, low-potency ingredients, or ineffective forms that the body can’t absorb.
Here are a few ways you can find effective supplements:
1. Look for Third-Party Testing and Certifications
Choose brands that verify the purity, potency, and safety of their products through independent labs. Look for seals like:
- USP Verified (United States Pharmacopeia)
- NSF Certified
- ConsumerLab.com Approved
These certifications test for contaminants like heavy metals, verify label accuracy, and confirm ingredient identity.
2. Choose Bioavailable Forms
Some nutrient forms are far better absorbed and utilized by the body than others. For example:
- Magnesium glycinate is more calming and absorbable than magnesium oxide.
- Methylcobalamin (B12) is preferable to cyanocobalamin, especially for individuals with MTHFR mutations
- Methylfolate is more effective than folic acid for those with impaired methylation.
- Curcumin (the active ingredient in turmeric) is best absorbed when paired with piperine (black pepper extract) or formulated as a liposomal or phytosomal complex.
3. Avoid Common Red Flags
Be wary of supplements that:
- Rely on proprietary blends without disclosing exact dosages
- Contain artificial dyes, titanium dioxide, or unnecessary fillers
- Are marketed as “cure-alls” or use sensationalist language
Avoid buying supplements from unverified online marketplaces. Instead, purchase directly from trusted companies or through professional-grade distributors.
4. Dose Smartly, Test Often
More isn’t always better. Fat-soluble vitamins (A, D, E, K) can accumulate, and even water-soluble ones (like B6) can cause side effects at high doses. Your coursework emphasizes that supplements should follow lab testing and individualized protocols when possible
Conclusion
Navigating perimenopause can feel like riding a hormonal rollercoaster—unpredictable, exhausting, and often overwhelming. But with the right foundation of nutrition, lifestyle habits, and evidence-based perimenopause supplements, it is absolutely possible to reclaim balance, energy, and clarity during this transformative stage.
From foundational nutrients like magnesium, B vitamins, and omega-3s to targeted support for hot flashes, mood swings, low libido, and brain fog, supplements can offer strategic relief when used appropriately. Addressing gut health and estrogen metabolism—through tools like probiotics, DIM, and glutamine—adds another layer of powerful support, particularly for women experiencing estrogen dominance or post-pill symptoms.
At the same time, caution is crucial. Not all supplements are safe or necessary for every woman. Products like DHEA and fat-soluble vitamins must be approached with care and ideally under the guidance of a qualified practitioner. Quality matters as much as content: well-sourced, bioavailable, third-party-tested products are essential for both safety and efficacy.
Ultimately, supplements are support tools, not silver bullets. Their true value emerges when used in conjunction with personalized care, proper testing, and attention to the whole woman—not just her hormone levels. Be curious, cautious, and empowered—and always remember that this is a time of transition, not decline.
Perimenopause is not just something to “get through.” With the right tools, it can be a powerful opportunity for healing, clarity, and renewal.
