Perimenopause and cortisol are deeply interconnected, and understanding their relationship can help women navigate this important life stage with greater ease.

Perimenopause marks the transitional years before menopause, bringing hormonal shifts that impact nearly every system in the body. At the same time, cortisol—the body’s primary stress hormone—can become harder to regulate, leading to a wide range of symptoms like fatigue, weight gain, anxiety, and sleep disturbances.
This blog post explores how the changes of perimenopause influence cortisol levels, how cortisol imbalances show up during this time, and most importantly, how women can support their bodies through the transition.
What is Perimenopause?
Perimenopause is the transitional phase leading up to menopause, typically beginning in a woman’s late 30s or 40s. It can last anywhere from a few years to over a decade, depending on the individual. During this time, the ovaries gradually produce less estrogen and progesterone—the key hormones that regulate the menstrual cycle and many other bodily functions.
The hormonal fluctuations of perimenopause are not linear; they often happen in unpredictable waves. One month, hormone levels might be relatively stable; the next, they might swing dramatically, creating symptoms that can feel confusing and overwhelming.
Common signs of perimenopause include irregular periods, hot flashes, night sweats, mood swings, sleep disturbances, brain fog, and changes in weight distribution, particularly an increase in belly fat.
Understanding the hormonal chaos of perimenopause sets the stage for appreciating how cortisol, the stress hormone, can be thrown further off balance during this life stage.
What is Cortisol and Why Does It Matter?
Cortisol is a vital hormone produced by the adrenal glands that plays a central role in the body’s response to stress. Often referred to as the “stress hormone,” cortisol helps regulate a wide range of processes, including blood sugar levels, metabolism, inflammation, immune response, and even memory formation.
Under normal circumstances, cortisol follows a daily rhythm: it peaks in the early morning to help you wake up and get energized, then gradually declines throughout the day, reaching its lowest levels at night to promote restful sleep. This natural cycle supports energy, mood, focus, and recovery.
However, when the body experiences chronic stress—or when other hormonal systems, like those affected during perimenopause, become disrupted—cortisol production can go awry. Levels may stay elevated when they should fall, or become too low when the body needs energy and alertness. Both patterns of imbalance can significantly affect how women feel and function during perimenopause.
Understanding cortisol’s wide-ranging influence is key to appreciating why perimenopausal hormonal shifts can feel so destabilizing.
How Perimenopause Impacts Cortisol Levels
Perimenopause and cortisol are closely linked because of the dramatic hormonal shifts that occur during this transitional phase. One major change is the decline in progesterone, a hormone that not only supports reproductive health but also acts as a natural buffer to cortisol. As progesterone levels fall, women may find themselves more sensitive to stress and less able to “bounce back” from everyday challenges.
Estrogen, another key hormone that fluctuates and eventually declines during perimenopause, also has important interactions with cortisol. Estrogen helps regulate the hypothalamic-pituitary-adrenal (HPA) axis—the system that controls the body’s stress response. When estrogen levels drop, the HPA axis can become more reactive, leading to exaggerated cortisol surges even in response to minor stressors.
Additionally, sleep disturbances, common in perimenopause due to night sweats or hormonal shifts, can further elevate cortisol levels. Poor sleep creates a feedback loop: higher cortisol disrupts sleep, and disrupted sleep raises cortisol even more.
This complex hormonal interplay explains why many women in perimenopause report feeling more anxious, exhausted, and overwhelmed than they did in earlier stages of life.
Symptoms of Cortisol Imbalance in Perimenopausal Women
Perimenopause and cortisol imbalances can create a cascade of symptoms that affect both physical and emotional well-being. Because cortisol touches so many systems in the body, its dysregulation during perimenopause can manifest in ways that might initially seem unrelated.
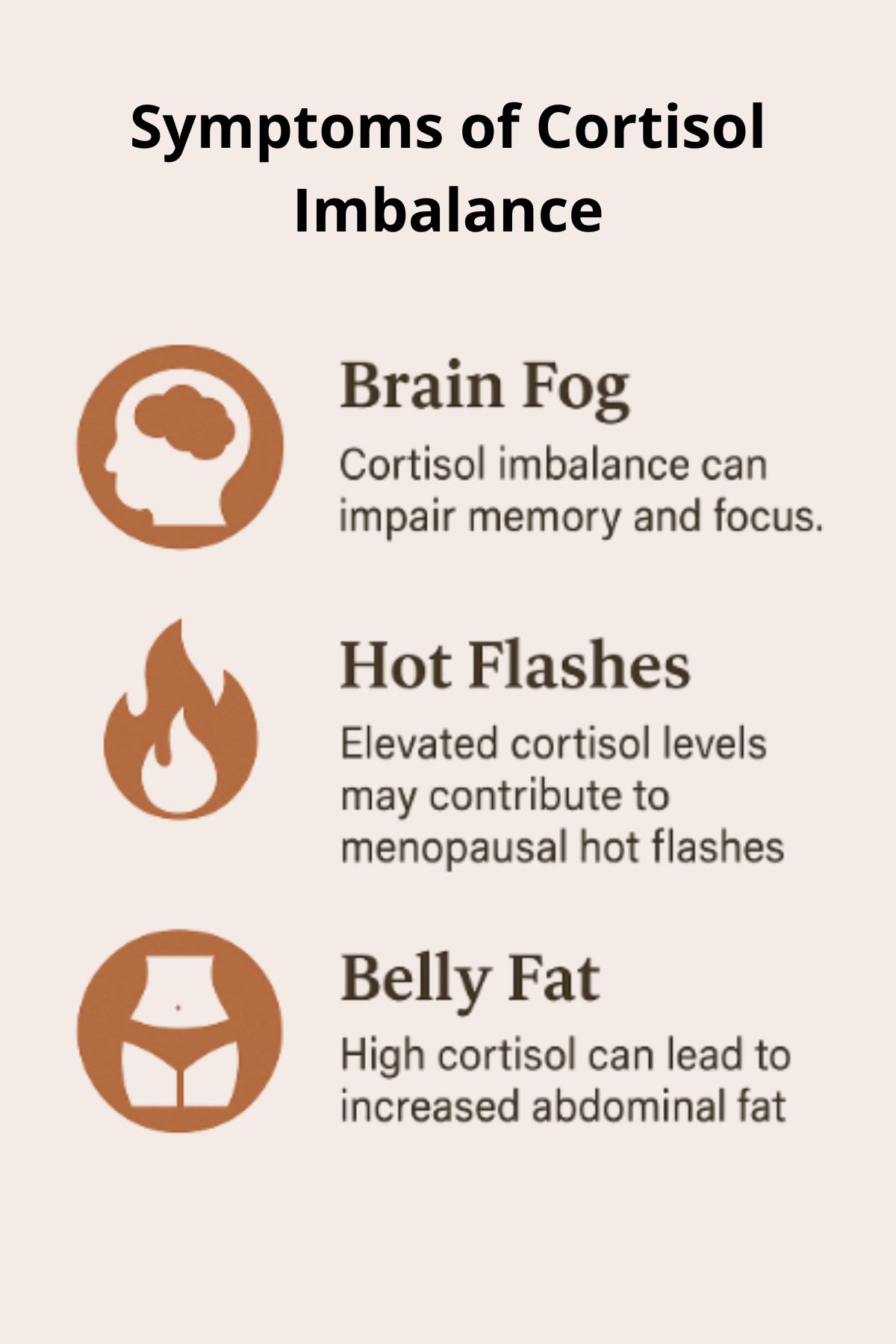
Some of the most common symptoms include:
- Sleep Disturbances: Difficulty falling asleep, frequent nighttime awakenings, or waking up feeling unrefreshed are hallmark signs of cortisol disruption.
- Anxiety and Mood Swings: Women may experience heightened feelings of anxiety, irritability, or emotional volatility, even if they previously managed stress well.
- Weight Gain, Especially Around the Midsection: Elevated cortisol promotes fat storage, particularly visceral fat, leading to an increase in belly weight that feels resistant to diet and exercise.
- Fatigue and Low Energy: Despite sleeping for adequate hours, women often feel chronically tired, a sign that cortisol rhythms are out of sync.
- Blood Sugar Instability: Cortisol plays a critical role in regulating blood glucose. Imbalances can cause cravings for sugar or salty foods, energy crashes between meals, and even shakiness or irritability.
Recognizing these symptoms as potential signs of cortisol imbalance—not just “getting older”—is the first step toward reclaiming health and vitality during perimenopause.
Long-Term Health Risks of Cortisol Dysregulation
While the day-to-day symptoms of cortisol imbalance can be frustrating, the long-term effects—especially during perimenopause—deserve just as much attention. Chronic cortisol dysregulation can quietly set the stage for more serious health conditions over time.
Here are some of the key long-term risks:
- Insulin Resistance and Type 2 Diabetes: Persistently high cortisol levels raise blood glucose and impair insulin sensitivity. Over time, this can lead to insulin resistance—a key driver of type 2 diabetes, especially for women in midlife.
- Cardiovascular Disease: Cortisol can increase blood pressure, raise LDL cholesterol, and promote systemic inflammation—all risk factors for heart disease, the leading cause of death in women.
- Osteoporosis and Bone Loss: Cortisol inhibits bone-building cells and decreases calcium absorption, accelerating bone loss, which is already a concern post-menopause due to declining estrogen.
- Cognitive Decline and Brain Fog: Elevated cortisol over the long term has been linked to memory issues, brain shrinkage in key areas, and increased risk for dementia.
- Weakened Immune Function: Chronic stress and elevated cortisol can suppress the immune system, making the body more vulnerable to infections and slower to heal.
These risks underscore why it’s not just about feeling better today—managing cortisol during perimenopause is an investment in long-term health and resilience.
How to Support Healthy Cortisol Levels During Perimenopause
Managing cortisol during perimenopause isn’t about eliminating stress completely—it’s about improving the body’s ability to respond to and recover from it. Because the hormonal landscape is shifting, small, consistent strategies can have a powerful impact.
1. Prioritize Restorative Sleep
- Aim for 7–9 hours of quality sleep each night.
- Establish a calming bedtime routine—dim lights, limit screens, and avoid stimulants late in the day.
- Magnesium glycinate, herbal teas (like chamomile), or gentle yoga can support sleep naturally.
2. Balance Blood Sugar with Every Meal
- Include protein, fiber, and healthy fats to reduce cortisol spikes triggered by blood sugar crashes.
- Avoid skipping meals or over-relying on caffeine and sugar to push through the day.
3. Choose the Right Kind of Movement
- Swap high-intensity workouts for cortisol-friendly options like walking, Pilates, light strength training, or dancing.
- Gentle movement reduces stress and supports hormone balance without overwhelming the adrenals.
4. Build Daily Stress-Relief Rituals
- Practice mindfulness, deep breathing, or meditation—even 5 minutes helps.
- Journaling, time in nature, creative hobbies, and connection with loved ones also buffer cortisol.
5. Consider Adaptogens (with Guidance)
- Herbs like ashwagandha, rhodiola, and holy basil may help regulate cortisol, but should be used under the guidance of a knowledgeable practitioner—especially in the context of perimenopause.
6. Set Boundaries and Honor Your Limits
- Learn to say no to unnecessary obligations.
- Recognize that your body may need more recovery time than it used to—and that’s not a weakness.
Supporting healthy cortisol rhythms during perimenopause isn’t about perfection—it’s about tuning into your body’s needs and giving it what it has always deserved: rest, nourishment, and compassion.
When to Seek Help
Perimenopause and cortisol symptoms can often be managed with lifestyle changes, but there are times when professional support is not only helpful—it’s essential. If symptoms begin to interfere with your daily life, relationships, or overall well-being, it’s a signal to reach out for guidance.
Consider seeking help if you experience:
- Persistent sleep problems despite healthy habits
- Ongoing anxiety, panic attacks, or mood swings
- Unexplained weight gain or inability to lose weight
- Extreme fatigue that doesn’t improve with rest
- Brain fog or memory lapses that affect work or personal life
- Irregular or unusually heavy menstrual cycles
Perimenopause and Cortisol: Conclusion
Perimenopause and cortisol are intricately linked, and understanding their connection is key to navigating this life stage with greater resilience and vitality. As hormonal shifts during perimenopause naturally alter the body’s stress response, women may find themselves facing new challenges like disrupted sleep, increased anxiety, stubborn weight gain, and persistent fatigue.
The good news is that small, intentional changes—like supporting sleep, balancing blood sugar, managing stress, and seeking professional help when needed—can make a significant difference. By tuning into your body’s signals and honoring its needs, you can ease the transition through perimenopause and set the foundation for long-term health and well-being.
Remember: you are not alone, and with the right strategies and support, this can be a time of empowerment, renewal, and strength.
