Itching and perimenopause often go hand in hand, yet many women are surprised to find themselves dealing with persistent skin irritation as they transition through midlife. While hot flashes, irregular periods, and mood swings get most of the attention, itching—whether it’s dry, prickly, or inexplicably persistent—is a symptom that deserves more recognition. As hormone levels shift, particularly estrogen and progesterone, a variety of changes can occur that affect skin health, detoxification, and even nervous system sensitivity.
For some women, the discomfort is mild and fleeting. For others, itching becomes a frustrating, even distressing part of their perimenopausal journey. What makes this issue more complex is that the causes are often layered—ranging from declining estrogen to toxin accumulation to nutritional deficiencies that develop subtly over time. This article will explore the root causes of itching during perimenopause and provide practical, holistic strategies for relief—covering everything from detoxification and nutrient balance to hormone-safe skincare and gut health.
Understanding Perimenopause and Skin Changes
Perimenopause is the transitional phase leading up to menopause, often beginning in a woman’s 40s, though it can start earlier or later. During this time, the body undergoes significant hormonal fluctuations—particularly in estrogen and progesterone—that impact nearly every system, including the skin.
Estrogen plays a vital role in maintaining skin hydration, elasticity, and thickness. It stimulates the production of collagen, natural oils, and hyaluronic acid—key components that keep skin smooth and supple. As estrogen levels begin to decline in perimenopause, the skin loses moisture more easily, becomes thinner, and may take longer to heal. This increased fragility can make the skin more prone to irritation, dryness, and ultimately, itching.
Another lesser-known connection is histamine sensitivity. Estrogen influences how the body breaks down histamine—a chemical involved in allergic reactions and inflammation. As hormonal balance shifts, some women become more sensitive to histamine, which can cause or intensify itching, even in the absence of an obvious allergen or rash.
The combination of estrogen deficiency, impaired barrier function, and shifting inflammatory responses helps explain why itching and perimenopause are so often linked—yet so frequently misunderstood.
What Causes Itching in Perimenopause?
The causes of itching in perimenopause are often multifactorial, involving a complex interplay between hormonal imbalances, nutrient deficiencies, environmental exposures, and detoxification pathways. Understanding these contributors can help identify effective strategies for relief.
Hormonal Triggers
Estrogen, a key hormone that declines during perimenopause, plays a crucial role in skin function. It promotes collagen production, maintains moisture, and regulates inflammation. When estrogen levels drop, the skin becomes drier, thinner, and more reactive. Reduced progesterone may also contribute by affecting skin cell turnover and water retention.
Additionally, fluctuating hormones can influence histamine regulation. Estrogen inhibits the enzyme that breaks down histamine, so during perimenopause, women may become more reactive to histamine, even from foods or environmental sources that never caused issues before—leading to itchy, inflamed skin.
Nutritional Deficiencies
Micronutrients and healthy fats are essential for skin health and nervous system regulation. Deficiencies that are common during perimenopause can make itching worse:
- Vitamin A supports skin renewal and immune protection.
- Vitamin D helps modulate inflammation and immunity.
- Zinc and magnesium reduce histamine reactions and support barrier function.
- Omega-3 fatty acids, especially EPA and DHA, help calm inflammation and maintain the skin’s lipid barrier.
When the intake or absorption of these nutrients is inadequate—as often happens due to stress, poor diet, or digestive issues—the skin becomes more vulnerable to dryness and itching.
Environmental and Chemical Triggers
Daily exposure to endocrine-disrupting chemicals (EDCs)—such as parabens, phthalates, triclosan, and BPA—can interfere with hormonal balance and irritate the skin. These chemicals are commonly found in personal care products, plastics, cleaning supplies, and even clothing. They may mimic estrogen, block hormone receptors, or overload detox organs, creating systemic inflammation and sensitivity.
This internal and external burden can manifest as mysterious itching—especially in women already experiencing the hormonal shifts of perimenopause.
Gut and Liver Detoxification Link
The body eliminates toxins and excess hormones through the liver and gut. But during perimenopause, sluggish digestion, reduced bile flow, and constipation can impair detoxification, allowing toxins and estrogens to recirculate. This toxic buildup can trigger systemic inflammation, and in some cases, the skin becomes the outlet for elimination—resulting in itching, rashes, or hives.
Supporting gut health with fiber, probiotics, and hydration, and reducing processed foods and alcohol, can significantly ease the burden on the detox pathways—and the skin.
Where Itching Occurs Most Often
Itching during perimenopause can show up in unexpected places, often without visible rashes or irritation. Understanding the most commonly affected areas can help women recognize hormonal itching and distinguish it from other causes like allergies or dermatologic conditions.
Arms, Legs, and Back
These areas are common sites for generalized dry skin (xerosis) due to reduced oil production. Women may notice flaky patches, tightness after showering, or a persistent need to scratch—especially at night or in dry climates.
Chest and Neck
The skin here is thinner and more sensitive to heat, fabrics, and perfumes. Fluctuations in estrogen and histamine can cause localized itching, especially in the evening or after consuming histamine-releasing foods like red wine or aged cheese.
Scalp
Dryness or changes in hair care products can aggravate scalp itching. Hormonal changes may also impact sebum production, contributing to dryness, dandruff, or increased sensitivity to shampoo ingredients.
Underarms and Skin Folds
These areas may be affected by sweat, synthetic fabrics, or deodorants containing aluminum and fragrance. As skin becomes more sensitive, products that were once well-tolerated may suddenly cause stinging, itching, or redness.
Vulvar and Vaginal Area
This is a unique and often distressing site of itching during perimenopause, driven by declining estrogen and thinning of the vaginal mucosa. This topic is covered more extensively in Section 6 due to its distinct causes and treatment needs.
Because itching and perimenopause can affect different regions of the body for different reasons, paying attention to location-specific triggers and sensations can help guide targeted relief strategies.
Hidden Toxins in Your Daily Routine
One of the most overlooked contributors to itching during perimenopause is daily exposure to environmental toxins—particularly those that disrupt hormones or irritate the skin. These compounds, known as endocrine-disrupting chemicals (EDCs), are found in many common products and can interfere with the delicate hormonal balance already shifting during this life stage.
Personal Care Products
Soaps, lotions, shampoos, perfumes, and cosmetics often contain ingredients like:
- Parabens – preservatives that mimic estrogen
- Phthalates – used to enhance fragrance and texture
- Triclosan – an antibacterial agent that disrupts thyroid function
- Benzophenones – found in sunscreens and linked to skin sensitivity and hormone disruption
When applied directly to the skin, these substances may not only trigger surface irritation but also be absorbed into the bloodstream, compounding internal hormonal chaos and contributing to itching and inflammation.
Plastics and Food Packaging
Plastic containers, cling wrap, and even the linings of canned goods can leach BPA and similar xenoestrogens into food and drinks. Heating food in plastic dramatically increases this risk. These compounds mimic estrogen and may amplify estrogen dominance symptoms or confuse hormone receptors—leading to symptoms like itchy skin, PMS, and fatigue.
Cleaning and Air Freshening Products
Common household cleaners, synthetic air fresheners, and laundry detergents often release volatile organic compounds (VOCs), which are known respiratory and skin irritants. Continuous low-level exposure can trigger histamine release, low-grade inflammation, and sensitization over time.
Clothing and Fabrics
Many women experience itching in areas where tight or synthetic fabrics contact the skin—especially underarms, waistbands, and bra lines. Flame retardants, chemical dyes, and non-breathable materials may be at fault. Choosing organic cotton, bamboo, or OEKO-TEX® certified fabrics can reduce exposure to skin-irritating chemicals.
By becoming more aware of these hidden sources of irritation and hormonal disruption, women can take steps to reduce their toxic load and give the skin—and the endocrine system—a chance to recalibrate.
Vaginal and Vulvar Itching
Among the most uncomfortable and emotionally distressing symptoms of perimenopause is vaginal and vulvar itching. While less openly discussed, this type of itching is extremely common and is often caused by hormonal changes that directly affect the tissues of the genital area.
The Role of Estrogen
Estrogen maintains the thickness, elasticity, and moisture of vaginal and vulvar tissues. As levels drop during perimenopause, these tissues begin to thin, dry out, and become more sensitive—a condition known as genitourinary syndrome of menopause (GSM). The result can be persistent itching, burning, tightness, or discomfort during intimacy.
Common Symptoms
- Dryness or a sandpaper-like feeling
- Burning or stinging—especially during urination
- Persistent or intermittent itching
- Pain or irritation during intercourse
- Increased susceptibility to infections or irritation from hygiene products
Irritants That Worsen Symptoms
Even products once tolerated may begin to cause problems during this stage. Common culprits include:
- Scented soaps, pads, and toilet paper
- Tight or synthetic underwear
- Bubble baths or vaginal wipes
- Lack of lubrication during intercourse
Supportive Solutions
Fortunately, there are safe and effective solutions for relief:
- Topical vaginal moisturizers used regularly
- Natural lubricants like aloe-based or water-based formulas
- Vaginal estrogen therapy prescribed in very low doses; often safe even for women who can’t take systemic hormones
- Probiotics to support the vaginal microbiome
- Cotton underwear and loose, breathable clothing
- Avoidance of scented or antibacterial hygiene products
Addressing genital itching requires a gentle, targeted approach that restores moisture and supports tissue repair. Recognizing it as a valid and manageable part of the broader picture of itching and perimenopause helps reduce stigma and ensures women seek the care they need.
Lifestyle Strategies for Relief
When addressing itching and perimenopause, quick fixes rarely work. What does work is a comprehensive lifestyle approach that supports hormonal balance, strengthens the skin barrier, and reduces internal and external triggers. The good news? Small, consistent changes can make a significant difference.
Nutrition and Hydration
- Anti-inflammatory foods like leafy greens, berries, fatty fish, flaxseed, and chia support skin repair and calm immune responses.
- Omega-3-rich foods such as sardines, wild salmon, walnuts, and pasture-raised eggs help strengthen the skin’s lipid barrier and reduce inflammation.
- Hydration is essential. Aim for filtered water and herbal teas throughout the day to support detox pathways and prevent skin dehydration.
- Fiber-rich foods like lentils, avocados, and cruciferous vegetables support bowel regularity, which is essential for hormone and toxin elimination.
Detoxification Support
- Epsom salt baths, infrared saunas, and sweating through movement help eliminate toxins through the skin.
- Cruciferous vegetables (like broccoli, kale, and Brussels sprouts) contain compounds that support estrogen detoxification in the liver.
- Use natural deodorants, phthalate- and paraben-free skincare, and glass or stainless-steel food containers to reduce toxic burden.
- Consider dry brushing or gentle exfoliation to support lymphatic flow and improve skin texture.
Key Supplements (Always consult a practitioner)
- Vitamin D: Supports immune and skin health; deficiency is common in perimenopause.
- Magnesium: Calms nerves, reduces histamine reactions, and supports hydration at the cellular level.
- Zinc: Supports barrier repair and reduces inflammation.
- Fish oil or algae oil supplements: To boost omega-3 intake if dietary sources are lacking.
- Milk thistle or dandelion root: To support liver function and hormone metabolism.
Skincare Habits
- Use fragrance-free, hypoallergenic moisturizers containing ceramides or colloidal oatmeal.
- Shower in lukewarm (not hot) water and apply moisturizer immediately afterward.
- Avoid exfoliating too aggressively, especially on sensitive areas.
Adopting these daily habits can gradually reduce the intensity and frequency of itching. While results may take time, this approach addresses the underlying contributors rather than simply masking symptoms.

When to Seek Medical Help
While itching and perimenopause are often related to natural hormonal shifts and lifestyle factors, it’s important to know when symptoms may point to something more serious. Persistent or unusual itching should never be ignored, especially if it interferes with daily life or worsens over time.
Red Flags That Warrant Evaluation
- Itching that lasts longer than 2–3 weeks, even with moisturizing and lifestyle changes
- Itching accompanied by visible rash, sores, blisters, or broken skin
- Itching that disrupts sleep or daily activities
- Itching that worsens despite avoiding irritants
- Vaginal or vulvar itching with discharge, odor, or bleeding
Potential Underlying Conditions
Certain medical issues may mimic or exacerbate hormonal itching:
- Hypothyroidism – Common in midlife and linked to dry, itchy skin
- Liver dysfunction – Can cause generalized itching due to bile salt buildup
- Kidney disease – Often results in widespread itching
- Allergic dermatitis or eczema – May flare more during perimenopause
- Infections – Yeast or bacterial vaginosis can present with vulvar itching
What to Expect from a Provider Visit
- A thorough history of your symptoms, cycle, and lifestyle
- Physical exam of the affected areas
- Possible lab tests for thyroid, liver, kidney function, or nutrient levels
- Recommendations for topical or prescription treatments if needed
Seeking help doesn’t mean something is wrong—it simply ensures that you’re addressing every possible factor. For many women, combining professional guidance with holistic strategies leads to faster and more complete relief.
Key Takeaways
Itching and perimenopause are more closely connected than many women realize. What may seem like an isolated skin issue is often a reflection of deeper hormonal shifts, detoxification challenges, nutrient deficiencies, and daily exposures to irritants and endocrine disruptors.
Here are the key insights to remember:
- Hormonal fluctuations, particularly declining estrogen, can thin the skin, increase dryness, and make the body more reactive to histamine and stress—contributing to persistent itching.
- Micronutrient deficiencies, especially in vitamin A, vitamin D, zinc, and omega-3 fatty acids, are common in perimenopause and play a central role in skin barrier integrity and inflammation control.
- Endocrine-disrupting chemicals in skincare, plastics, and household products can mimic or interfere with hormones, intensifying symptoms like itching, especially in hormonally sensitive areas.
- Gut and liver detox pathways often slow down in midlife, which can increase the internal burden of toxins and estrogens that would otherwise be eliminated—leading to skin flare-ups.
- Stress and sleep deprivation can amplify itching by raising cortisol levels, delaying skin repair, and creating a cycle of inflammation and hypersensitivity.
- Lifestyle interventions such as anti-inflammatory nutrition, low-toxin living, gentle detox support, and consistent skincare can offer meaningful, long-lasting relief.
By approaching itching and perimenopause with a holistic mindset, women can begin to address the root causes instead of just treating the symptoms. Empowerment comes from understanding the “why” behind the discomfort—and taking proactive steps toward hormonal and skin health.
FAQs
How to Stop Perimenopause Itching
To stop perimenopause-related itching, it’s important to address both internal root causes and external triggers. Here’s a step-by-step approach:
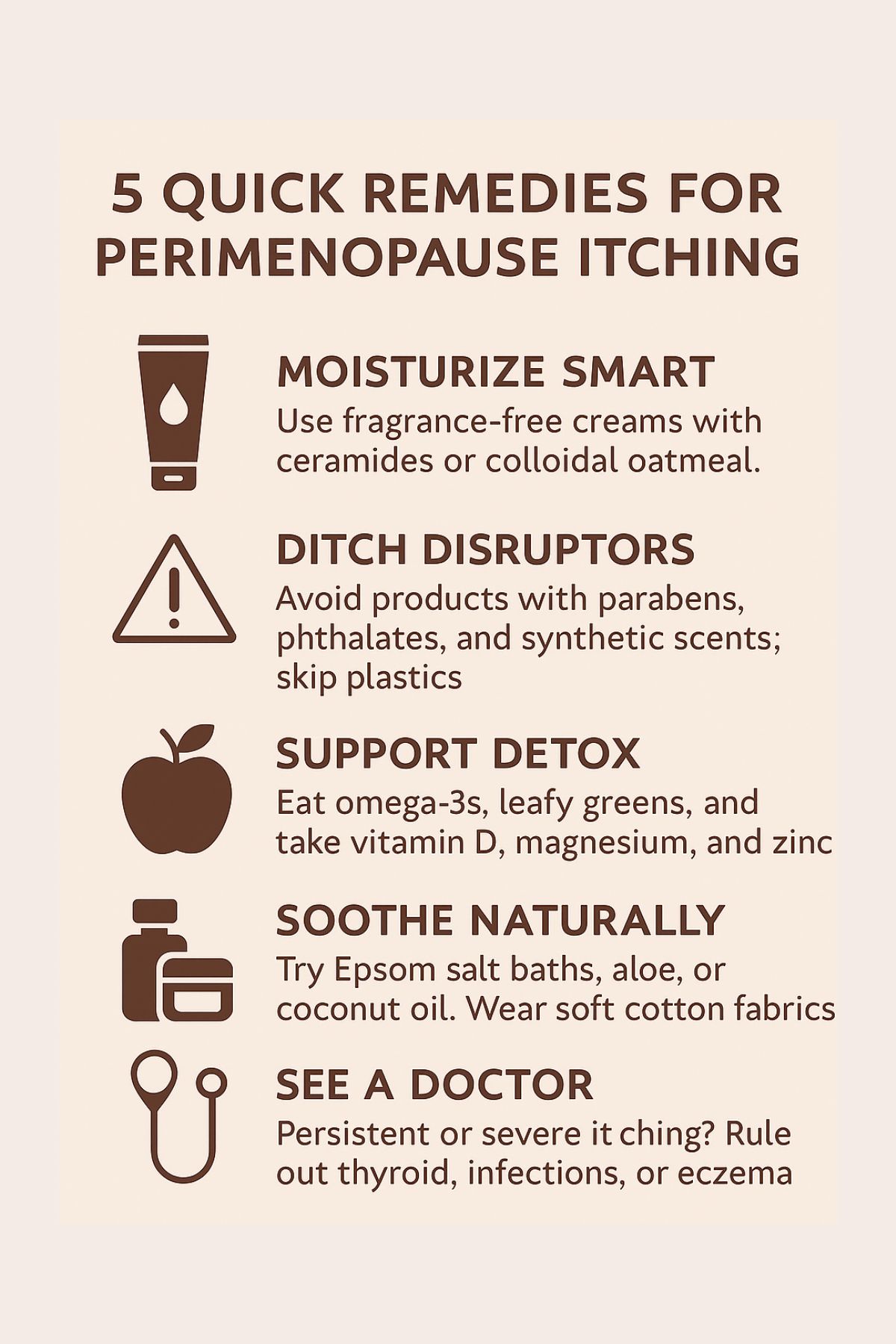
✅ 1. Rehydrate and Repair the Skin
- Use fragrance-free, hypoallergenic moisturizers containing ceramides, colloidal oatmeal, or hyaluronic acid.
- Apply moisturizer immediately after showering to lock in hydration.
- Avoid hot showers and harsh soaps that strip natural oils.
✅ 2. Balance Hormones Naturally
- Declining estrogen is a key cause of dry, itchy skin. Support hormonal balance by:
- Managing stress (to reduce cortisol)
- Getting quality sleep
- Considering vaginal estrogen (for genital itching) or bioidentical hormone therapy under medical guidance
✅ 3. Eliminate Endocrine Disruptors
- Swap out skincare, makeup, and cleaning products that contain parabens, phthalates, triclosan, and synthetic fragrances.
- Avoid plastics (especially when heating food), and choose glass or stainless steel instead.
✅ 4. Support Detox and Gut Health
- Eat fiber-rich foods (like flaxseed, lentils, leafy greens) to help your body clear excess estrogen and toxins.
- Drink plenty of filtered water.
- Consider liver-supporting herbs like milk thistle and dandelion root.
- Address constipation, which can worsen itching by impairing elimination.
✅ 5. Replenish Key Nutrients
- Supplement or increase intake of:
- Omega-3s (salmon, sardines, flaxseed oil)
- Vitamin D, magnesium, and zinc
- Vitamin A from food sources (e.g., leafy greens, sweet potato)
✅ 6. Soothe Itching Naturally
- Try Epsom salt baths, aloe vera gel, or coconut oil for external relief.
- Avoid synthetic fabrics and wear breathable cotton clothing.
✅ 7. Know When to Seek Help
- If itching is severe, persistent, or accompanied by a rash or discharge, consult a healthcare provider to rule out other causes like thyroid imbalance, eczema, or infections.
