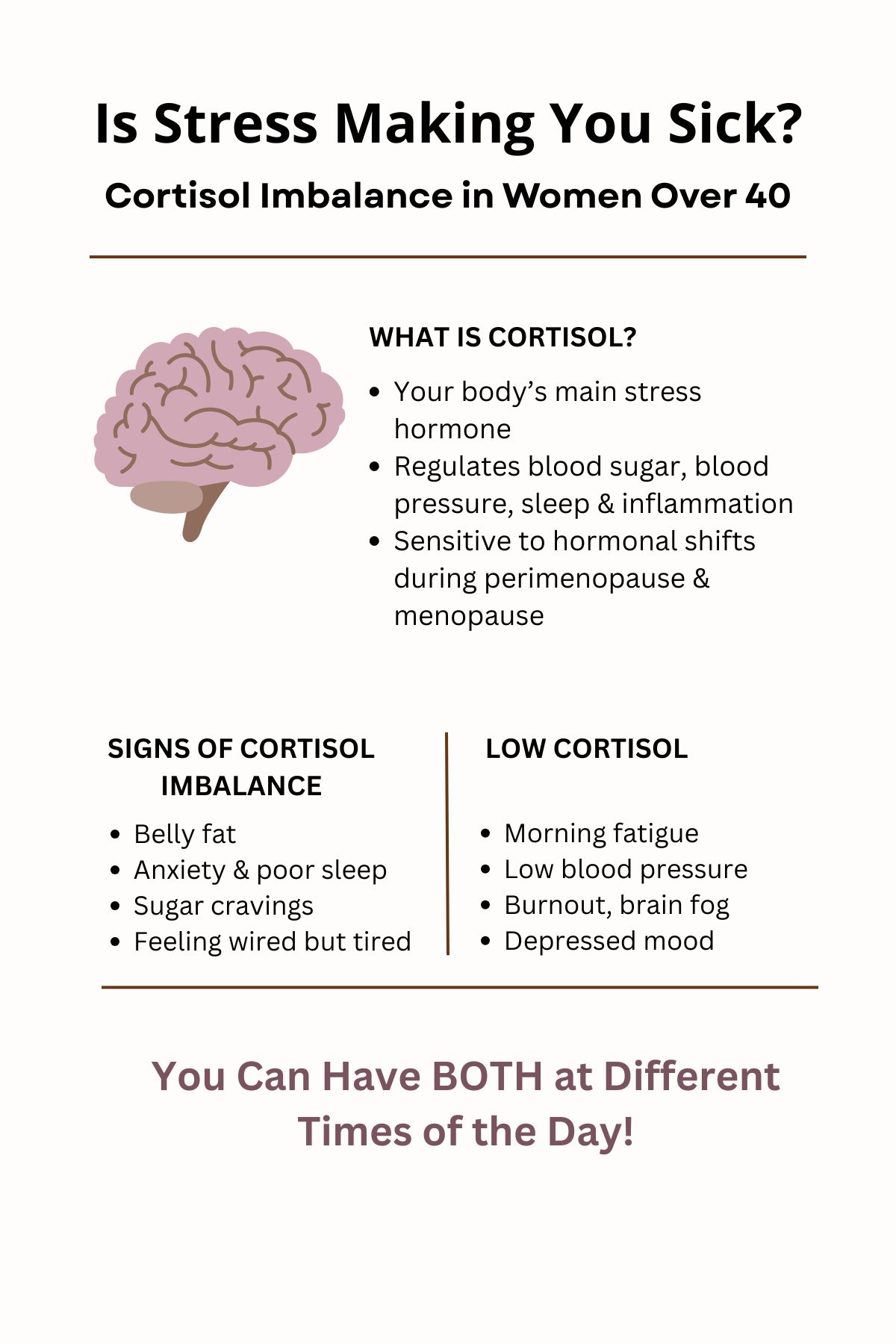
Cortisol imbalance is one of the hidden reasons why so many women over 40 feel exhausted, anxious, and unable to bounce back from everyday stress. Cortisol is your body’s primary stress hormone—produced by your adrenal glands in response to physical, emotional, or environmental stress. It’s a crucial part of your survival toolkit, helping regulate your blood sugar levels, blood pressure, inflammation, immune function, digestion, and even your sleep-wake cycle. In short, cortisol is meant to keep you alive during a crisis.
But as women enter perimenopause (the years leading up to menopause) and menopause, the way your body manages cortisol can dramatically change. Estrogen and progesterone—two key hormones that help buffer the stress response—start to decline. Without their stabilizing effects, cortisol becomes harder to regulate. What was once a normal, temporary stress reaction can now turn into chronic cortisol imbalance.
Normally, cortisol rises in the morning to help you wake up, drops gently throughout the day, and is at its lowest during the night to allow for restful sleep. This natural rhythm is called your diurnal cortisol pattern. However, for many women over 40, chronic stress combined with hormonal changes flattens or inverts this pattern—leading to symptoms like fatigue, insomnia, weight gain, brain fog, and mood swings.
Additionally, cortisol belongs to a hormone family called glucocorticoids, whose primary job is to maintain stable blood sugar by increasing glucose production and storing it in the liver. When cortisol is chronically high—as it often is during the turbulent years of perimenopause—your blood sugar levels stay elevated, raising your risk for prediabetes and type 2 diabetes.
Understanding cortisol is especially critical after 40, when the natural aging process plus hormonal shifts make women more vulnerable to stress-related breakdowns in metabolism, immune function, and mental health. Recognizing the signs of cortisol imbalance early—and taking proactive steps—can dramatically improve your energy, mood, weight, and overall quality of life during the menopause transition and beyond.
Cortisol Imbalance Symptoms
Recognizing the symptoms of cortisol imbalance is crucial—especially during perimenopause and menopause, when hormonal shifts amplify your body’s vulnerability to stress. The tricky part is that cortisol dysregulation can present in two very different ways: as high cortisol or low cortisol. Even more confusing, many women experience both extremes in the same day.
Let’s break it down:
High Cortisol Symptoms
When cortisol levels are too high for too long, your body stays stuck in “fight-or-flight” mode. Common signs include:
- Stubborn belly fat, even with a healthy diet and exercise
- Anxiety, irritability, and feeling constantly on edge
- Difficulty falling asleep, or waking up between 2–4 a.m.
- High blood pressure
- Sugar cravings and increased appetite
- Memory problems and brain fog
- Feeling “wired but tired” — exhausted yet unable to relax
During perimenopause, estrogen fluctuations can worsen cortisol spikes, making anxiety, irritability, and sleep disturbances even more intense.
Low Cortisol Symptoms
Over time, after years of elevated stress, your adrenal glands can become depleted. This leads to low cortisol, also called adrenal fatigue or burnout. Symptoms include:
- Morning fatigue (even after a full night’s sleep)
- Low blood pressure (feeling dizzy when standing up)
- Depression, emotional flatness, or feeling detached
- Frequent infections or slower wound healing
- Salt cravings
- Low resilience to everyday stressors
- Lack of motivation and loss of joy
This pattern is often seen in women after years of managing chronic stressors—caregiving, careers, parenting teens, financial worries—all while navigating the physical changes of menopause.
You Can Have Both at Once
It’s important to know that cortisol is dynamic—it’s not just “high” or “low.” Many women experience:
- High cortisol at night → making it hard to fall asleep
- Low cortisol in the morning → making it hard to wake up refreshed
This inverted rhythm disrupts your body’s ability to rest, repair, and balance other hormones like insulin, estrogen, and progesterone. Left unchecked, it contributes to accelerated aging, weight gain, and emotional burnout.
Knowing these signs is the first step toward reclaiming your health. If you recognize yourself in several of these symptoms, it’s worth exploring whether cortisol imbalance could be the hidden driver behind how you’re feeling.
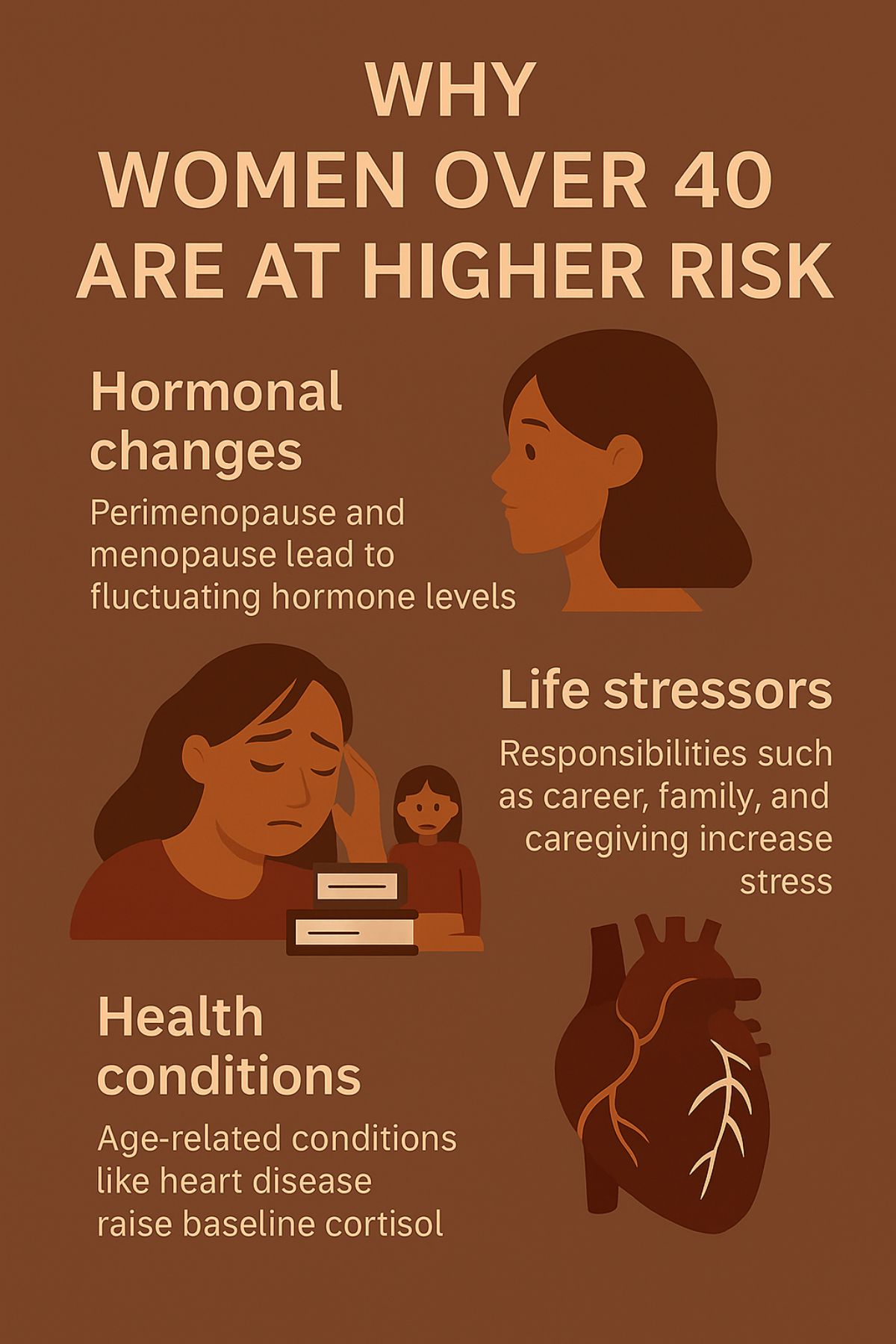
Why Women Over 40 Are More at Risk
After the age of 40, many women find that the strategies they once used to “push through” stress no longer work. This isn’t a matter of willpower or resilience—it’s biology. The hormonal shifts of perimenopause and menopause fundamentally change the way a woman’s body responds to stress, making cortisol balance more fragile than ever.
Here’s why women over 40 are particularly vulnerable:
1. Decline in Estrogen and Progesterone
Estrogen and progesterone play a powerful role in buffering the effects of cortisol. Estrogen helps enhance the calming effects of oxytocin (the “love and bonding” hormone), while progesterone naturally has a sedating, anxiety-reducing effect on the brain.
As these hormone levels begin to fluctuate and decline during perimenopause and menopause, cortisol’s effects can become more pronounced. Without hormonal “shock absorbers,” women experience greater mood swings, anxiety, sleep disturbances, and weight gain in response to even mild stress.
2. Shift from Fight-or-Flight to Tend-and-Befriend
Women’s stress responses differ biologically from men’s. Instead of only fighting or fleeing, women often engage the “tend-and-befriend” response—seeking social connection to cope with stress. This behavior is fueled by oxytocin, which rises when women spend time with trusted friends or family.
However, modern life often isolates women just when they need connection most. Between busy work schedules, caregiving for aging parents, and managing households, opportunities to “tend and befriend” diminish—causing cortisol to stay elevated.
3. Increased Allostatic Load
Allostatic load refers to the “wear and tear” on the body from chronic stress. As women juggle careers, relationships, parenting, and aging parents, the cumulative effect takes a toll. Research shows that women between 35 and 50 report the highest levels of stress-related health issues—including poor sleep, digestive problems, and mood disturbances—all linked to cortisol dysregulation.
Without regular periods of recovery, women’s adrenal glands become overtaxed, leading eventually to low cortisol and burnout.
4. Aging Itself Raises Cortisol
Even without external stress, cortisol levels naturally increase with age. Studies show a rise in cortisol levels between the ages of 50 and 89. Meanwhile, the body’s cells become less sensitive to cortisol’s actions, meaning cortisol remains elevated in the bloodstream but less effective inside cells.
This imbalance creates a vicious cycle: feeling tired and wired at the same time, even if outward stress seems manageable.
When you layer hormonal changes, life pressures, and biological aging together, it’s no wonder so many women over 40 struggle with unexplained fatigue, stubborn weight, emotional swings, and cognitive fog. Recognizing these changes is the first step toward healing—and reclaiming a vibrant second half of life.
How Cortisol Imbalance Impacts Your Health
When cortisol stays imbalanced—either chronically high, chronically low, or swinging wildly throughout the day—it doesn’t just make you tired or stressed. It reshapes your health at a cellular level, accelerating aging, increasing disease risk, and undermining your hormonal stability, especially during perimenopause and menopause.
Here’s how cortisol imbalance can wreak havoc:
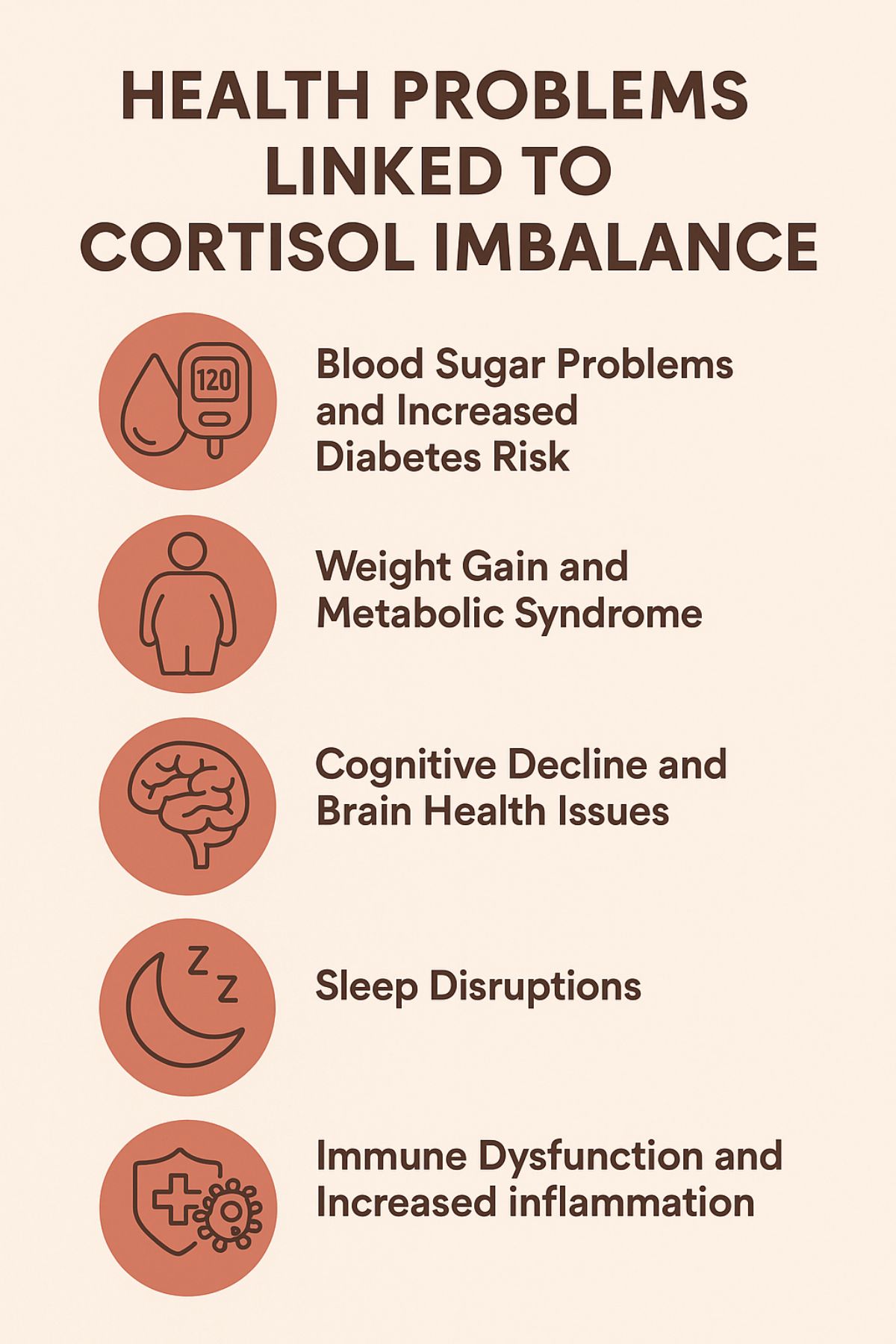
1. Blood Sugar Problems and Increased Diabetes Risk
Cortisol’s primary job is to raise blood sugar during times of stress to give you quick energy. But when cortisol is elevated all the time, your blood sugar stays high even when you don’t need it.
Over time, this leads to insulin resistance, prediabetes, and eventually type 2 diabetes—a trend that becomes much more common after age 40, particularly during and after menopause.
2. Weight Gain and Metabolic Syndrome
High cortisol makes your body store fat, especially around the midsection. This stubborn “menopause belly” isn’t just frustrating—it’s dangerous. Belly fat is hormonally active tissue that produces more inflammatory signals, worsening cortisol dysregulation.
Many women over 40 develop metabolic syndrome: a cluster of high blood pressure, high triglycerides, low HDL (“good” cholesterol), elevated blood sugar, and a thick waistline (over 35 inches). This significantly raises the risk for heart disease and stroke.
3. Cognitive Decline and Brain Health Issues
Chronically high cortisol literally shrinks parts of your brain, particularly the hippocampus, which is responsible for memory and learning.
Over time, women with elevated cortisol levels have a greater risk of:
- Memory problems
- Mood disorders (like depression and anxiety)
- Earlier onset of cognitive decline and dementia, including Alzheimer’s disease
Managing cortisol is not just about feeling better—it’s about preserving brain function long-term.
4. Sleep Disruptions
If cortisol is elevated at night (instead of its natural low point), it can cause:
- Difficulty falling asleep
- Waking up frequently during the night
- Feeling unrefreshed in the morning, even after “enough” sleep
Poor sleep further dysregulates cortisol, creating a vicious cycle that is very common in perimenopausal and menopausal women.
5. Immune Dysfunction and Increased Inflammation
Cortisol normally helps control inflammation. But when it’s out of balance, the immune system either overreacts (causing more inflammation) or underreacts (leaving you more vulnerable to infections).
This imbalance can worsen:
- Autoimmune conditions
- Chronic fatigue
- Fibromyalgia
- Slow wound healing
6. Bone Loss and Fracture Risk
High cortisol levels are linked to bone density loss, particularly in postmenopausal women who are already at increased risk for osteoporosis. Elevated cortisol weakens the structure of your bones, raising the risk of hip fractures and vertebral fractures later in life.
In short: if left unaddressed, cortisol imbalance can silently drive many of the health struggles women face after 40—including those often blamed on “normal aging” or “just menopause.” The good news is, with the right interventions, you can rebalance cortisol—and protect your long-term vitality.
Why Doctors Often Miss the Signs
Despite how common cortisol imbalance is among women over 40—especially during perimenopause and menopause—it often goes completely undiagnosed. Many women are told that their symptoms are “normal,” “just aging,” or worse, that it’s all in their head.
Here’s why cortisol issues are so often missed in mainstream healthcare:
1. Conventional Medicine Looks Only for Extremes
Most traditional doctors are trained to diagnose severe cortisol disorders like Cushing’s syndrome (extremely high cortisol) or Addison’s disease (dangerously low cortisol).
But subclinical cortisol imbalances—the milder, more common dysfunctions—don’t fit neatly into these categories. If your labs aren’t “extreme,” your symptoms may be dismissed, even though you’re struggling with fatigue, insomnia, weight gain, or anxiety.
2. Standard Testing Is Rarely Ordered
Cortisol testing is not part of routine annual physicals. Unless there’s a glaring clinical reason (like a tumor), doctors typically don’t check:
- Salivary cortisol (important for detecting daily rhythms)
- Diurnal cortisol patterns (how cortisol rises and falls throughout the day)
- Low-grade adrenal dysfunction (early signs of adrenal burnout)
3. Symptoms Are Misattributed to Menopause or Depression
It’s true that perimenopause and menopause come with hormonal changes—but cortisol dysfunction often layers on top of estrogen and progesterone decline, making symptoms worse.
Yet many women reporting fatigue, mood swings, or weight gain are quickly prescribed:
- Antidepressants
- Sleep medications
- Hormone replacement
…without ever checking if cortisol imbalance is a root cause.
This can lead to partial or no improvement—and missed opportunities to restore true hormone balance.
4. Cortisol Dysregulation Is a “Gray Zone”
Unlike cholesterol or blood pressure, there’s no universally agreed-upon number for what constitutes “too high” or “too low” cortisol unless it’s extreme.
This “gray zone” leaves many women untreated because their numbers look normal on paper, even though they feel completely off.
5. Gender Differences Are Overlooked
Most historical research on the stress response was conducted on men. Only in recent decades have we begun to understand that women’s stress responses—and their biological vulnerability to cortisol imbalance during midlife hormonal shifts—are different and unique.
Ignoring this gender-specific reality leaves many women underdiagnosed and undertreated at exactly the time when cortisol management could have the greatest impact on healthy aging.
👉 Bottom line: If you feel that something isn’t right—especially as you move through perimenopause or menopause—trust your instincts. Persistent fatigue, sleep problems, stubborn weight gain, and mood shifts deserve a deeper look at cortisol function, not just surface-level symptom control.
How to Fix Cortisol Imbalance
If you’re recognizing yourself in the symptoms and patterns we’ve discussed so far, the good news is: you have options. Cortisol imbalance—whether it shows up as too high, too low, or a daily roller coaster—can be improved significantly with a targeted, step-by-step approach.
Here’s where to start:
1. Cortisol Imbalance Test
Before jumping into supplements or drastic changes, it’s important to test, not guess. The most helpful tests for assessing cortisol levels include:
- Saliva cortisol tests (especially four-point diurnal testing across the day)
- Dried urine tests (DUTCH tests) for comprehensive hormone panels
- Blood cortisol tests (less ideal for daily rhythm but useful in some cases)
Tip: If you’re still menstruating, test around day 21–22 of your cycle for more accurate comparisons. Hormone fluctuations around ovulation can otherwise affect cortisol readings.
Testing provides a clear picture of whether you’re dealing with high cortisol, low cortisol, or a disrupted cortisol rhythm—and allows for a customized plan.
2. Track Your Symptoms
Even without testing, paying close attention to your symptoms can give valuable clues. You might notice:
- Waking up tired but wired at night
- Crashing mid-afternoon
- Craving sugar, salt, or caffeine
- Feeling emotionally fragile, anxious, or flat
- Difficulty coping with even small stressors
A daily symptom journal can help you (and your healthcare provider) spot patterns and measure improvement over time.
3. Reset Your Lifestyle Foundations
Before reaching for supplements or hormone therapy, focus on rebuilding your lifestyle habits—because cortisol is highly sensitive to your environment.
Key areas to address:
- Nutrition: Focus on blood sugar stability (e.g., protein-rich breakfasts, reduced refined carbs, anti-inflammatory foods)
- Sleep hygiene: Aim for 7–9 hours of restful sleep; avoid screens and stress triggers at night
- Movement: Gentle, rhythmic exercise like walking, yoga, or swimming (high-intensity workouts can worsen high cortisol if overdone)
- Breathwork and mindfulness: Practices like diaphragmatic breathing, meditation, and progressive muscle relaxation lower cortisol naturally
Small changes add up—and are the foundation for hormone balance after 40.
4. Consider Adaptogens and Supplements (Carefully)
Once your lifestyle reset is underway, targeted support can help, but it’s important to match the right strategy to your cortisol pattern.
For example:
- High cortisol: Ashwagandha, Rhodiola, phosphatidylserine, fish oil
- Low cortisol: Licorice root, vitamin C, B vitamins, adaptogens like maca
Always start supplements under the guidance of a practitioner familiar with adrenal and hormone health, especially during perimenopause and menopause when other hormone levels are shifting.
5. Heal Your Relationship with Stress
Perhaps the most powerful—and underrated—strategy is changing how you perceive and manage stress.
Even small shifts can retrain your brain and body to respond differently:
- Cultivate a “modular mindset” (break problems into smaller parts)
- Prioritize daily joy and connection (the oxytocin boost helps regulate cortisol)
- Practice gratitude or forgiveness (both scientifically shown to lower stress hormones)
- Set boundaries around technology and work
- Remember: Stress isn’t just external—it’s also how we interpret and react to life’s demands.
Conclusion
If you’re a woman over 40 who feels exhausted by life’s demands—struggling with sleep, mood swings, stubborn weight gain, or a sense that your body just isn’t bouncing back like it used to—cortisol imbalance may be the missing piece.
As you move through perimenopause and into menopause, your hormones are in transition. This natural shift, layered with the chronic stress of modern life, creates the perfect storm for cortisol to spiral out of control. And when cortisol is off, it doesn’t just affect how you feel—it alters how your body functions, from blood sugar and brain health to immunity and aging.
But here’s the empowering truth: cortisol isn’t the enemy—chronic, unrelieved stress is.
And once you understand what’s happening, you can take control.
By getting clear on your symptoms, testing when needed, and rebuilding key lifestyle habits, you can support your body’s stress response, restore your energy, and feel more like yourself again.
This isn’t about fixing everything overnight. It’s about learning to recognize the signs your body is sending you—and giving it the support it needs to heal.
