Extreme fatigue in perimenopause can feel like hitting a wall you didn’t see coming—especially when your lifestyle hasn’t changed. One day you’re managing work, family, and responsibilities like always, and the next, even getting out of bed feels like a monumental task.
Perimenopause is the transitional phase leading up to menopause, marked by shifting hormone levels that can affect nearly every system in your body. While hot flashes and mood swings often take the spotlight, fatigue is a quieter but equally distressing symptom that’s frequently overlooked or misunderstood. Many women are told to “get more rest” or “manage stress,” without a deeper look at the root causes. Yet this fatigue is different—it doesn’t always resolve with sleep or downtime.
Understanding why this exhaustion occurs is the first step toward reclaiming your energy. In the sections that follow, we’ll break down the biological and lifestyle-related causes behind this symptom, how to recognize if it’s hormonally driven, and what you can do to restore vitality during this phase of life.
What Is Perimenopause?
Perimenopause is the hormonal transition period that typically begins in a woman’s late 30s or 40s and can last anywhere from several months to over a decade before menopause officially begins (defined as 12 consecutive months without a menstrual period). During this time, levels of estrogen and progesterone fluctuate unpredictably, which can lead to a wide range of physical, emotional, and cognitive symptoms.
One of the most commonly reported—and often underestimated—symptoms is fatigue. Women in perimenopause may experience sudden dips in energy, persistent tiredness, or difficulty recovering from daily exertion, even if they’re getting what used to be a sufficient amount of sleep.
In addition to extreme fatigue in perimenopause, many women notice other hallmark symptoms, including:
- Irregular or heavier periods
- Mood swings or irritability
- Anxiety or low mood
- Hot flashes and night sweats
- Brain fog or memory lapses
- Sleep disturbances
This constellation of symptoms can feel confusing and unpredictable. It’s not “just aging,” and it’s not in your head—it’s your body signaling that hormonal balance is shifting, and that it needs support.
Why Does Perimenopause Cause Extreme Fatigue?
Extreme fatigue in perimenopause is not simply the result of being “busy” or “getting older”—it’s a complex physiological response to multiple underlying changes in your body. Let’s break down the key contributors:
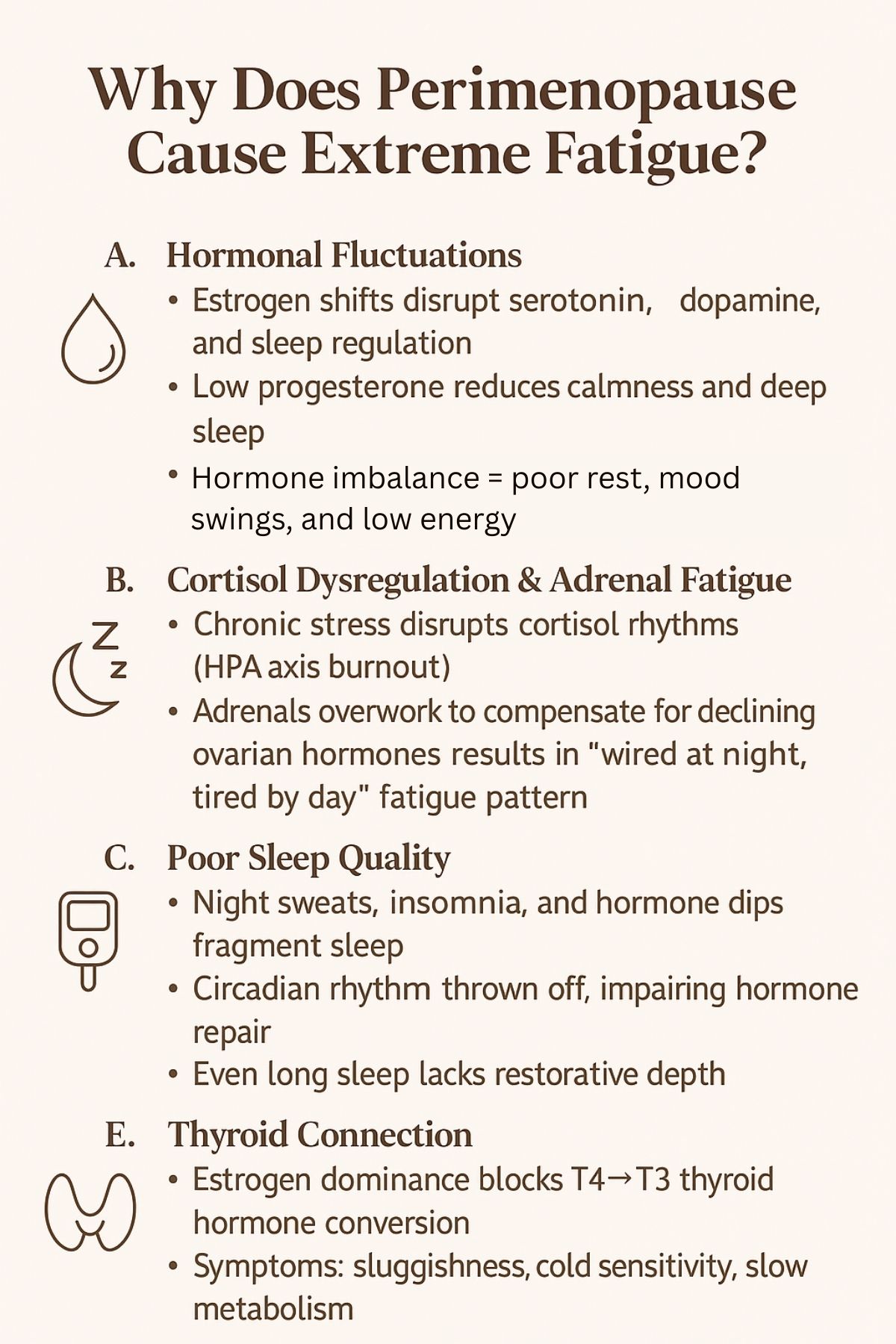
A. Hormonal Fluctuations
Estrogen and progesterone—your primary reproductive hormones—begin to rise and fall unpredictably during perimenopause. Estrogen plays a vital role in modulating serotonin, dopamine, and norepinephrine—neurotransmitters that regulate energy, mood, and sleep. When estrogen levels are erratic, so is your ability to feel rested and balanced.
Progesterone, often called the “relaxation hormone,” has a calming effect on the nervous system and promotes restful sleep. A drop in progesterone can result in anxiety, restlessness, and fragmented sleep—all of which contribute to fatigue.
B. Cortisol Dysregulation & Adrenal Fatigue
Chronic stress—emotional, physical, or metabolic—can dysregulate your hypothalamic-pituitary-adrenal (HPA) axis, the system responsible for managing cortisol output. During perimenopause, your body may lean more heavily on the adrenals to compensate for ovarian hormonal decline. If your stress response is overactive or depleted, you may feel “wired but tired”—alert at night and exhausted during the day.
Chronic stress pushes the body into survival mode, elevating cortisol levels and gradually reducing your ability to cope and recover. This state leads to flattened cortisol rhythms, low morning energy, and poor stress recovery.
C. Poor Sleep Quality
Sleep becomes more fragile in midlife. Night sweats, insomnia, and frequent nighttime waking due to fluctuating estrogen and progesterone levels disrupt the body’s natural circadian rhythm. Even if you’re in bed for 8 hours, fragmented sleep robs your body of the deep, restorative rest needed for cellular repair and hormone regulation.
D. Blood Sugar Imbalances
Estrogen helps improve insulin sensitivity, which stabilizes blood sugar. As estrogen declines, you may become more prone to glucose intolerance, leading to energy crashes, irritability, and sugar cravings. Eating high-glycemic meals or skipping meals can worsen the rollercoaster of fatigue and stimulation.
E. Thyroid Connection
Estrogen dominance (relative to low progesterone) can interfere with conversion of T4 to T3, the active form of thyroid hormone. The result? Low energy, cold intolerance, and sluggish metabolism. Because symptoms overlap—fatigue, weight gain, brain fog—thyroid dysfunction is often mistaken for a “normal” part of perimenopause.
How to Tell If Your Fatigue Is Hormonal
If you’re feeling constantly drained, you may wonder whether it’s your schedule—or your hormones. The truth is, extreme fatigue in perimenopause often has a distinct hormonal pattern that sets it apart from fatigue caused by poor sleep, iron deficiency, or overwork.
Here’s how to tell if your exhaustion may be hormonally driven:
1. Cyclical Fatigue
Hormonal fatigue often follows a cyclical rhythm, flaring up at certain points in your menstrual cycle—especially the luteal phase (after ovulation) or during anovulatory cycles when progesterone drops sharply. If your energy dips are worse in the days before your period, hormones are likely playing a role.
2. Poor Recovery After Rest
Unlike regular tiredness, hormonal fatigue doesn’t always improve with sleep or rest. You may get eight hours of sleep and still wake up foggy, heavy, and unrefreshed. This is a key clue that deeper systems like the HPA axis or thyroid may be involved.
3. Low Resilience to Stress
Perimenopausal women with cortisol dysregulation often feel overwhelmed by minor stressors or emotionally “fragile.” If you used to bounce back quickly but now feel emotionally wiped out by small disruptions, hormones could be affecting your adrenal resilience.
4. Other Hormonal Symptoms Are Present
If your fatigue is accompanied by symptoms like:
- Irregular cycles
- Night sweats
- Brain fog
- Weight gain (especially around the middle)
- Mood swings or anxiety
…then hormones are likely part of the picture.
5. Fatigue Worsens Around Menstrual Changes
The transition to menopause often includes skipped periods or months of unpredictable bleeding. These shifts in estrogen/progesterone balance can trigger dramatic drops in energy.
6. You Don’t Feel Like Yourself Anymore
Many women describe a sense of disconnection or depletion—like their body and brain aren’t working together. This type of fatigue can signal broader hormonal shifts impacting neurotransmitter balance, especially serotonin and dopamine.
What You Can Do About It
If you’re struggling with extreme fatigue in perimenopause, the good news is: you can support your energy and hormone balance with practical, evidence-based strategies. While there’s no one-size-fits-all fix, the following approaches address the root causes—rather than just managing symptoms.
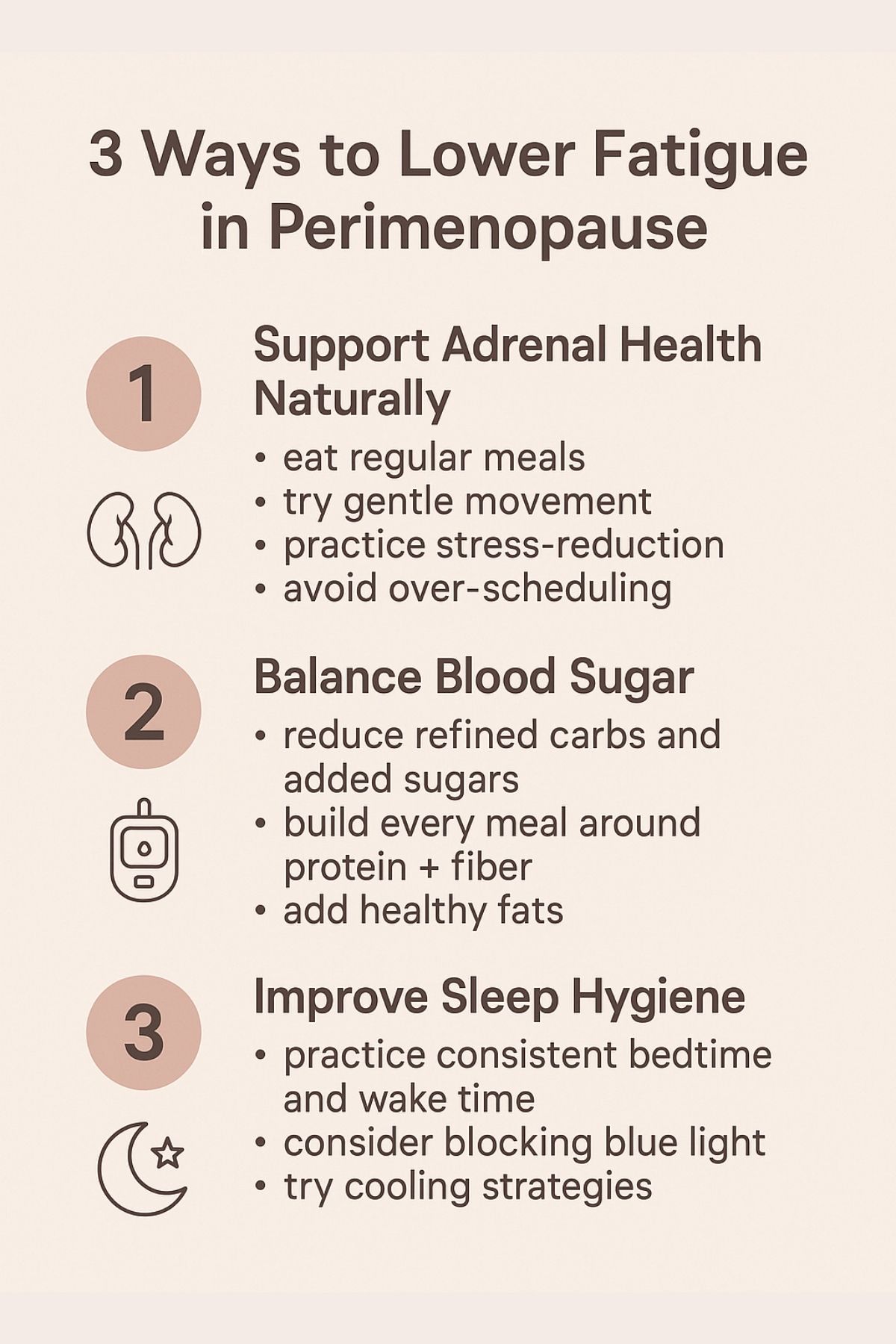
A. Support Adrenal Health Naturally
Your adrenal glands take on a bigger role in hormone production during perimenopause, especially when your ovaries slow down. Keeping your adrenals resilient can help stabilize energy, mood, and sleep.
- Eat regular meals: Avoid skipping meals or intermittent fasting if you’re depleted. Balanced meals with protein, fat, and complex carbs help reduce cortisol spikes.
- Gentle movement: Prioritize walking, yoga, Pilates, or short strength sessions.
- Be mindful of workout intensity: While movement is essential for hormone balance, high-intensity or prolonged exercise can backfire—especially if you’re already experiencing fatigue or stress. Intense workouts raise cortisol levels, which, when chronically elevated, can disrupt sleep, increase cravings, and suppress energy recovery. During perimenopause, your body may benefit more from restorative activities, especially in the second half of your cycle or during high-fatigue weeks. If a workout leaves you more drained than energized, it’s likely too much for your system right now.
- Stress-reduction practices: Daily breathwork, meditation, or even a short journaling session can help lower cortisol and calm your nervous system.
- Avoid over-scheduling: Build in rest—not just sleep—into your day to avoid burnout.
B. Balance Blood Sugar
Stable blood sugar is foundational to sustained energy and hormone balance.
- Reduce refined carbs and added sugars: These cause rapid spikes and crashes in glucose, triggering more fatigue.
- Build every meal around protein + fiber: This combination slows digestion, curbs cravings, and maintains energy.
- Add healthy fats: Avocados, nuts, seeds, and olive oil support hormone production and reduce post-meal glucose surges.
C. Improve Sleep Hygiene
Sleep is your hormonal reset button. Support better rest with:
- Consistent bedtime and wake time (even on weekends)
- Magnesium glycinate or topical magnesium to promote relaxation
- Blue light blocking or screen-free time 1 hour before bed
- Cooling strategies for night sweats: breathable bedding, fans, cooling sheets
Even if you can’t control night wakings, improving sleep quality can make a measurable difference in energy.
D. Consider Functional Testing
If fatigue persists despite lifestyle changes, testing may uncover hidden issues:
- Hormone panels: Look at estrogen, progesterone, DHEA, testosterone
- Cortisol rhythm tests: Saliva-based or DUTCH testing to assess adrenal patterns
- Thyroid labs: TSH, Free T3, Free T4, Reverse T3, and antibodies
- Ferritin and B12: Rule out anemia or nutrient deficiencies
- Vitamin D and Magnesium: Commonly low in women over 40 and critical for energy metabolism, immune function, and hormone regulation
Quick Note on Estrogen Dominance: This doesn’t always mean your estrogen levels are too high. More commonly in perimenopause, it means your progesterone levels are too low to balance estrogen, especially in cycles where ovulation doesn’t occur (anovulatory cycles). This relative imbalance can cause symptoms like fatigue, irritability, breast tenderness, water retention, and sleep disturbances—even if your estrogen levels are within a normal range.
Testing can provide clarity and guide targeted support rather than guessing.
Final Thoughts
If you’ve been feeling utterly drained and wondering what happened to your energy, know this: extreme fatigue in perimenopause is real—and you’re not imagining it. It’s one of the most common, yet least talked-about, symptoms women experience during this hormonal transition. You might look the same on the outside, but inside, your body is navigating major biochemical changes.
The good news? You have options. By understanding what’s happening physiologically and implementing small, consistent changes—nutritionally, emotionally, and with professional guidance—you can begin to restore balance. Listening to your body is the first step. If it’s asking for rest, nourishment, or a slower pace, that’s not weakness—it’s wisdom.
You don’t need to push through or “tough it out.” Instead, acknowledge this phase as an opportunity for deeper care and renewal. With the right support, many women not only regain energy but enter their post-menopausal years with greater clarity, strength, and purpose than ever before.
