Cortisol and progesterone are two powerful hormones that shape a woman’s mood, metabolism, and cycle health—especially after 40. But in today’s high-stress world, this delicate hormonal balance is easily disrupted.

You might feel tired but wired at night, experience more anxiety, struggle with weight gain, or notice your cycle becoming irregular. These aren’t just random symptoms—they’re signs that your body is prioritizing survival over balance.
In this article, we’ll explore how cortisol and progesterone interact, how chronic stress rewires hormonal pathways, the critical roles of gut health, inflammation, thyroid, and environment, and how to rebuild hormonal resilience through sustainable lifestyle shifts.
Meet the Players: Cortisol, Progesterone, and Estrogen
Cortisol – The Survival Hormone
Cortisol is your body’s primary stress hormone, released by the adrenal glands in response to physical, emotional, or environmental stress. It helps mobilize energy by raising blood sugar, increasing blood pressure, and suppressing systems deemed non-essential in a crisis—like digestion, reproduction, and immune function.
Short-term cortisol spikes help you respond to acute stress. But when stress becomes chronic, elevated cortisol can wreak havoc on other hormones, including progesterone. Over time, this leads to fatigue, sleep disruption, cravings, and difficulty managing weight.
Progesterone – The Calming Hormone
Progesterone is often called the “soothing” or “balancing” hormone. It’s primarily produced by the ovaries after ovulation and plays a key role in regulating the menstrual cycle, maintaining the uterine lining, and supporting mood and sleep.
Unlike cortisol, progesterone promotes calmness, counters the stimulating effects of estrogen, and helps you feel more grounded. But when cortisol dominates—especially in your 40s and beyond—progesterone often declines, amplifying stress-related symptoms and hormonal chaos.
The Role of Estrogen
While this article focuses on cortisol and progesterone, it’s important to recognize estrogen’s role. Low progesterone can create relative estrogen dominance—even if estrogen levels are normal. Estrogen dominance can worsen symptoms like heavy periods, bloating, breast tenderness, and mood swings.
How Stress Hijacks Hormonal Pathways
When stress becomes chronic, it doesn’t just make you feel frazzled—it reprograms how your hormones are made, delivered, and received. Cortisol, while essential in short bursts, becomes a disruptive force when it’s constantly elevated.
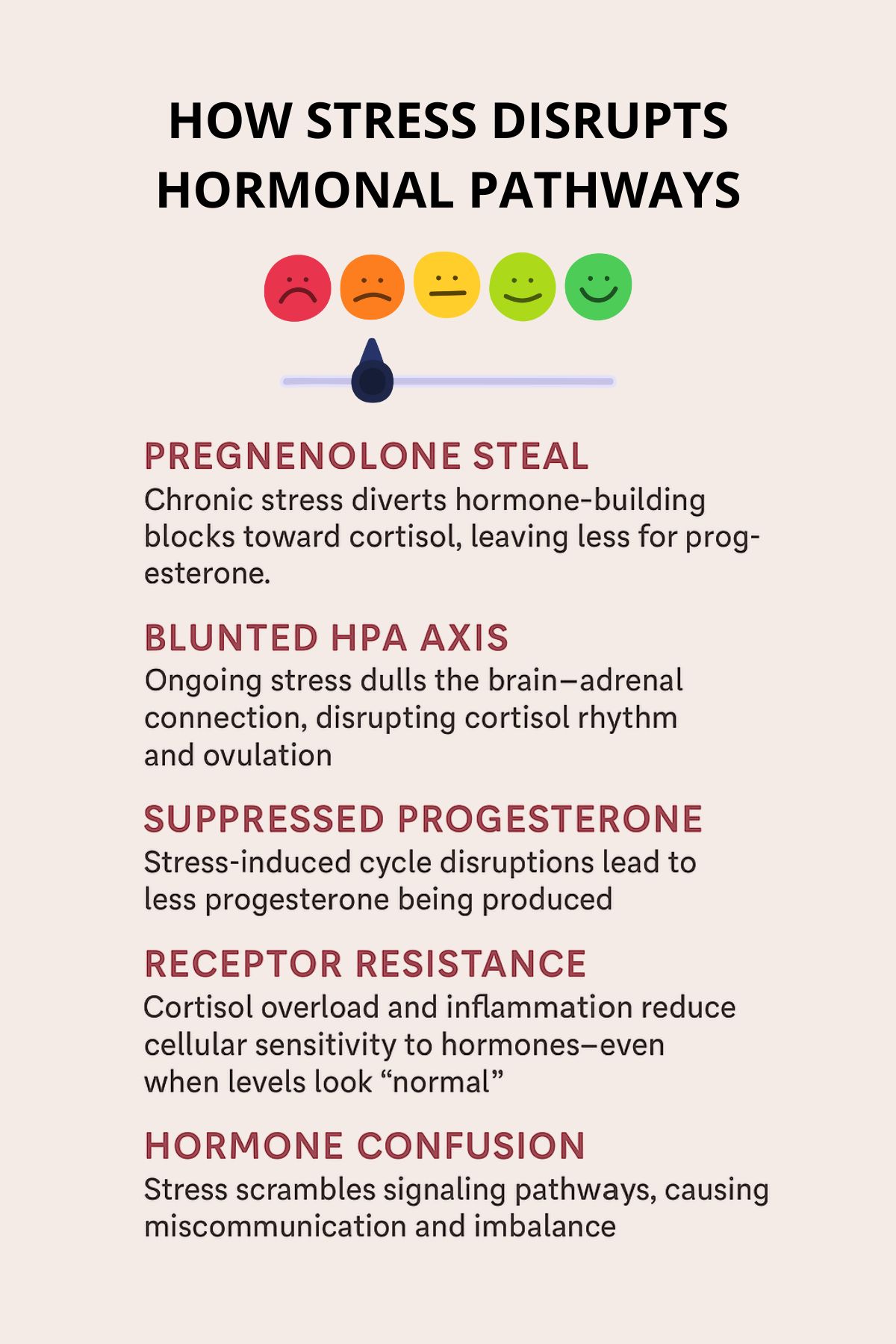
A. Pregnenolone Steal: When Cortisol Takes Priority
Your body uses a master hormone called pregnenolone as a starting material to produce many other hormones, including both cortisol and progesterone. Under chronic stress, the body diverts this raw material toward cortisol production, a phenomenon often called the “pregnenolone steal.”
The result? Less available pregnenolone to make progesterone. This means even if your ovaries are functioning normally, you might still experience low progesterone simply because your body is funneling resources toward surviving stress instead of supporting reproductive balance.
B. Disrupted HPA Axis and Hormone Signaling
The hypothalamic-pituitary-adrenal (HPA) axis is the command center that controls your stress response. Chronic activation—like daily emotional stress, poor sleep, or under-eating—can blunt this system’s sensitivity.
This results in:
- Flattened cortisol rhythms (e.g., low in the morning, high at night)
- Suppressed ovulation, which reduces progesterone output
- Miscommunication between the brain and adrenal glands, leading to hormone confusion
C. Receptor Resistance and Hormone Effectiveness
Even if your labs show “normal” progesterone or cortisol levels, your cells may not be responding properly. Cortisol overload can lead to receptor downregulation, where cells become less sensitive to hormones—much like what happens in insulin resistance.
Inflammation also interferes with hormone receptor function. When receptors are blocked or desensitized, hormones can’t carry out their jobs effectively, resulting in symptoms of hormonal imbalance despite standard test results.
Signs of Cortisol and Progesterone Imbalance
When cortisol and progesterone fall out of balance, your body sends signals—often subtle at first, then louder as the imbalance persists. These symptoms can show up cyclically or persistently, and many are mistakenly chalked up to “just aging” or “normal stress.”
Here are common signs that your stress hormone (cortisol) is overwhelming your calming hormone (progesterone):
- Irregular or short menstrual cycles
Chronic stress can interfere with ovulation, reducing progesterone production and shortening your luteal phase. - PMS, anxiety, or mood swings
Without enough progesterone to balance estrogen or buffer cortisol, you may feel edgy, emotional, or easily overwhelmed. - Difficulty falling or staying asleep
High evening cortisol and low progesterone both disrupt melatonin and sleep regulation. - Low libido and vaginal dryness
Hormonal depletion—especially of progesterone—can affect sexual desire and comfort. - Midsection weight gain
Cortisol encourages fat storage around the abdomen while lowering insulin sensitivity. - Cravings for sugar, salt, or caffeine
These are often your body’s cry for quick energy when your adrenals are struggling. - Breast tenderness or spotting before your period
Low progesterone relative to estrogen often triggers these symptoms.
If you’re noticing several of these signs, it could be your body’s way of telling you that stress is interfering with hormonal harmony.
Who’s Most at Risk
While anyone can experience cortisol-progesterone imbalance, certain groups of women are especially vulnerable—particularly during midlife transitions or in high-demand seasons of life.
1. Women in Perimenopause and Menopause
As ovarian function naturally declines, progesterone is the first hormone to drop—often years before estrogen significantly decreases. Combine this with the demands of modern life, and many women enter their 40s and 50s already hormonally disadvantaged. Even mild chronic stress can tip the balance further, making symptoms more pronounced.
2. High-Stress Lifestyles
Juggling work, family, caregiving, and personal goals leaves little room for rest. Women with “go-go-go” lives, poor sleep, or little downtime often have chronically elevated cortisol. Over time, this blunts ovulation and suppresses progesterone, leading to emotional and physical burnout.
3. Over-Exercisers or Under-Eaters
Women who overtrain or underfuel—especially those following restrictive diets or intense fitness regimens—may experience disrupted hormone production. The body views these as stressors, contributing to adrenal dysregulation and low progesterone levels.
4. Those with Trauma or Chronic Stress History
Unresolved trauma, childhood adversity, or long-term caregiving roles can lead to HPA axis dysfunction, where the stress system no longer responds appropriately. This can result in flattened cortisol rhythms and inadequate reproductive hormone signaling.
How to Regain Hormonal Balance
Rebalancing cortisol and progesterone isn’t about quick fixes—it’s about restoring communication between your brain, adrenals, and ovaries. The good news: small, consistent shifts in lifestyle and nutrition can have a profound impact.
A. Lower Cortisol Through Daily Rhythm Support
Cortisol is meant to follow a natural curve: high in the morning, tapering off by bedtime. Many women have the opposite due to poor sleep, blue light, or emotional overload. Recalibrating your daily rhythm is the foundation.
- Wake with natural light: 10–15 minutes of sunlight within 30 minutes of waking resets your cortisol rhythm.
- Consistent bedtime/wake time: Regulates both cortisol and melatonin.
- Avoid high-intensity workouts late at night: They can spike cortisol before bed.
- Create a wind-down ritual: Gentle yoga, journaling, or breathwork helps signal safety to the brain.
B. Re-Sensitize Hormone Receptors and Boost Progesterone Naturally
Restoring balance isn’t just about production—it’s also about receptor sensitivity. Nutrients, inflammation levels, and detox pathways all influence whether hormones work properly.
- Anti-inflammatory foods: Omega-3 fats (wild salmon, flax), cruciferous vegetables, turmeric, berries.
- Key nutrients:
- Magnesium glycinate – calms the nervous system and supports progesterone.
- Vitamin B6 – cofactor in progesterone synthesis.
- Vitamin C – nourishes adrenal glands.
- Adaptogens: Herbs like Rhodiola and Ashwagandha help regulate cortisol output and improve resilience.
C. Get the Right Tests
Testing gives you a map—not just hormone levels, but patterns.
- DUTCH Test (dried urine): Shows cortisol rhythm and progesterone metabolites.
- Saliva tests: Reveal bioavailable hormone levels across the day.
- Blood labs: Still useful, especially when paired with symptom tracking.
Ask your provider for mid-luteal progesterone testing (typically 5–7 days after ovulation) to assess true production levels.
D. Consider Targeted Hormone Support
Some women may benefit from natural or bioidentical support:
- Vitex (Chaste Tree): May gently increase luteal phase progesterone.
- Bioidentical progesterone cream: Used under supervision to ease perimenopausal symptoms.
- Support liver detoxification: Your liver helps break down used hormones. Support it with leafy greens, dandelion tea, and adequate hydration.
Environmental and Lifestyle Factors
Our hormones don’t exist in a vacuum. While internal imbalances like stress and nutrient depletion play a major role, external exposures and daily habits can have just as powerful an effect on your hormonal health. From the products in your bathroom cabinet to the way you move through your day, every choice you make sends a signal to your endocrine system. Understanding and adjusting these signals is a critical step in restoring balance.
Endocrine Disruptors: The Hidden Hormone Hijackers
Endocrine-disrupting chemicals (EDCs) are substances found in everyday items—plastics, pesticides, synthetic fragrances, cosmetics, canned foods, and cleaning products—that can mimic, block, or interfere with natural hormones like estrogen and progesterone. Over time, even low-level exposure can accumulate, leading to imbalances in reproductive hormones, thyroid function, and cortisol response.
To reduce exposure:
- Choose personal care products wisely: Look for EWG-verified, fragrance-free options made without parabens, phthalates, or triclosan.
- Switch to non-toxic cleaning products: Vinegar, baking soda, and castile soap are simple, hormone-safe alternatives.
- Avoid plastic food containers: Especially those labeled with #3, #6, or #7. Opt for glass, stainless steel, or ceramic.
- Filter your tap water: Many municipal supplies contain trace amounts of pesticides, heavy metals, and chlorine—all of which burden your detox systems.
- Buy organic when possible: Especially for the “Dirty Dozen” produce list to reduce pesticide load.
Making these small swaps over time can significantly lighten your body’s hormonal burden.
Inflammation’s Broader Impact on Hormones
Chronic inflammation—often fueled by stress, processed food, poor sleep, and toxic exposures—doesn’t just make you feel puffy or tired. It damages cellular receptors, alters hormone signaling, and keeps your nervous system in a state of high alert.
Left unchecked, systemic inflammation contributes to:
- Hormone receptor resistance (your body “stops listening” to progesterone and cortisol)
- Autoimmune flare-ups
- Cardiovascular disease and high blood pressure
- Brain fog, cognitive decline, and premature aging
- Insulin resistance and metabolic dysfunction
Reducing inflammation is about more than pain relief—it’s essential for protecting your hormone pathways and long-term health.
Sustainable Lifestyle Shifts: The Real Hormone Reset
There’s no magic pill or 3-day cleanse that can rebalance your hormones. Real healing comes from repeatable, realistic lifestyle choices—especially in a world that pushes us toward burnout.
Here’s what sustainable, hormone-supportive living looks like:
- Nourish consistently: Eat balanced meals with protein, fat, and fiber to stabilize blood sugar and support hormone production.
- Rest intentionally: Prioritize sleep, take breaks, and practice saying no without guilt.
- Move regularly—but not excessively: Gentle strength training, walking, and restorative yoga are powerful allies.
- Process emotions, don’t suppress them: Journaling, therapy, and breathwork help reset your nervous system.
- Reconnect with your body: Spend time in nature, practice self-touch, or simply check in with your breath.
Consistency—not perfection—is what builds resilience. Start with one or two shifts, and let them grow roots. Over time, these habits become the scaffolding for hormonal healing.
Potential Consequences of Chronic Imbalance
Hormonal symptoms like fatigue, anxiety, irregular cycles, and poor sleep are often treated as nuisances—but they’re actually early warning signals. When cortisol and progesterone remain imbalanced for extended periods, deeper health issues can begin to develop.
Here’s what may happen if this hormonal tug-of-war is left unchecked:
Osteoporosis and Bone Loss
Progesterone plays a protective role in bone-building by supporting osteoblast activity. Chronically low progesterone, especially during perimenopause and menopause, reduces bone density. Elevated cortisol further worsens the issue by leaching calcium from bones and impairing vitamin D metabolism—setting the stage for osteopenia or osteoporosis.
Heart Disease and Cardiovascular Risk
Cortisol influences blood pressure, cholesterol levels, and vascular tone. When chronically elevated, it contributes to hypertension, arterial inflammation, and insulin resistance. Meanwhile, low progesterone can worsen PMS-related palpitations and may contribute to poor sleep quality—both of which increase cardiovascular strain over time.
Insulin Resistance and Type 2 Diabetes
Cortisol raises blood glucose to help you “fight or flee.” But when it’s always elevated, cells stop responding properly to insulin, leading to blood sugar instability, cravings, belly fat, and eventually insulin resistance or even diabetes. Low progesterone may worsen blood sugar swings by impairing ovulatory function.
Thyroid Dysfunction
Chronic stress suppresses thyroid hormone conversion (T4 → T3) and slows thyroid hormone production altogether. Many women with high cortisol and low progesterone also experience hypothyroid symptoms like fatigue, cold intolerance, hair thinning, and brain fog—even if their labs look “normal.” This overlap often goes undiagnosed.
Mood Disorders: Anxiety and Depression
Progesterone has calming, mood-stabilizing effects via GABA receptor support. When levels are low—and cortisol is high—the result is often increased anxiety, irritability, and difficulty sleeping. Long-term imbalance can tip into clinical anxiety, panic attacks, or depression, especially during perimenopause.
Fertility Struggles and Cycle Irregularity
Progesterone is essential for maintaining the uterine lining and supporting early pregnancy. Cortisol-related cycle disruption (anovulation or luteal phase defects) can lead to infertility, recurrent miscarriage, or difficulty conceiving. Even for women not trying to conceive, cycle irregularity signals that the entire reproductive system is under stress.
Compounding Effects Over Time
These aren’t isolated issues—they often overlap and feed into each other. For example:
- Insulin resistance worsens inflammation
- Inflammation impairs thyroid function
- Thyroid dysfunction contributes to depression
- Depression elevates cortisol
- Elevated cortisol reduces progesterone
…and the cycle continues.
Why It Matters
Addressing cortisol-progesterone imbalance isn’t just about managing symptoms like PMS or fatigue—it’s about protecting your long-term vitality. Left unresolved, this imbalance can spiral into chronic disease, emotional burnout, and premature aging.
But the earlier you intervene, the more you can prevent, reverse, and rebuild.
Track Your Progress
Healing your hormones isn’t a one-size-fits-all process—it’s personal, dynamic, and nonlinear. That’s why tracking is one of the most powerful tools you can use to stay connected to your progress, symptoms, and patterns.
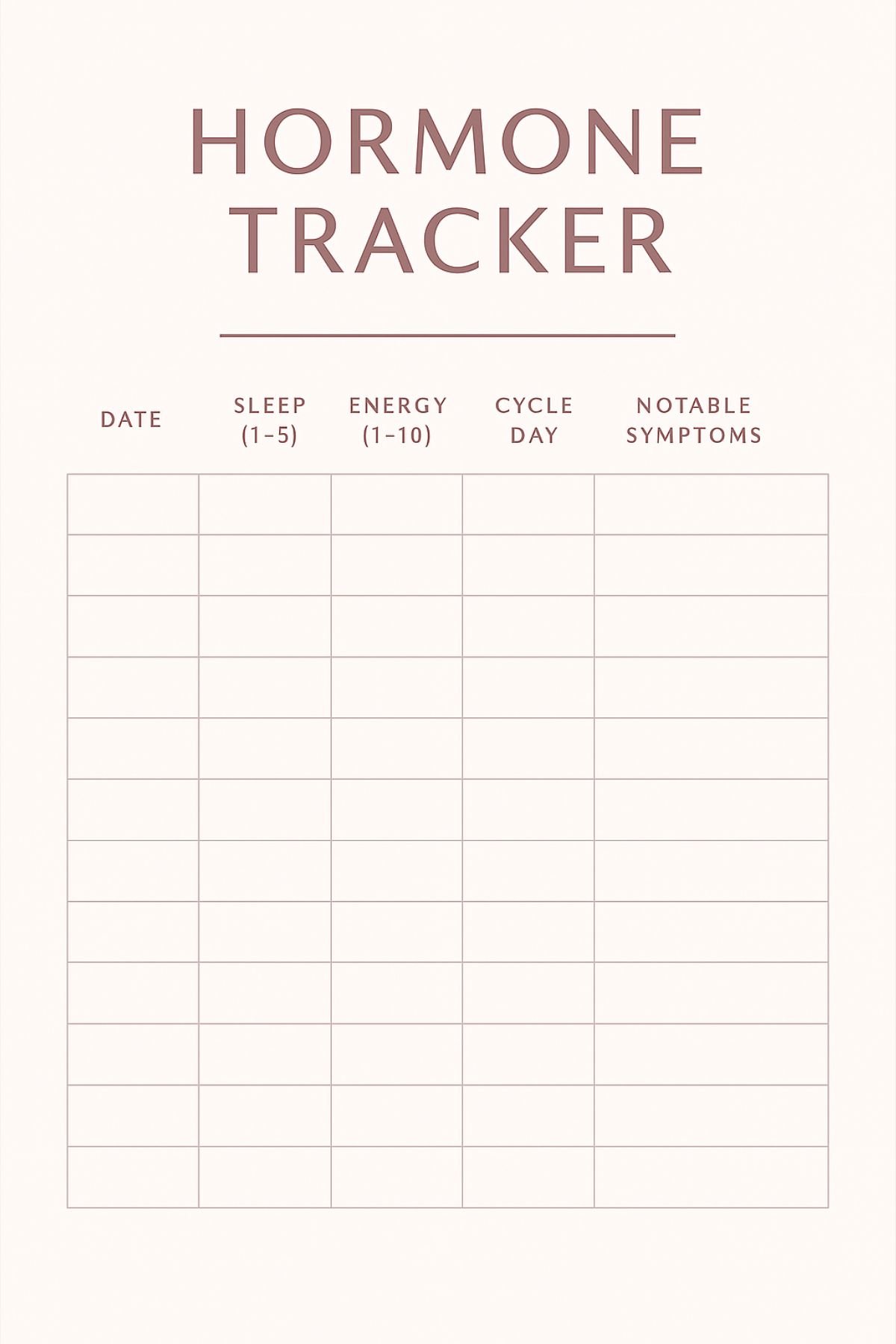
By observing how your body responds to stress, sleep, nutrition, and movement over time, you gain insight into what supports your balance and what disrupts it.
📖 How Long to Track
Start by committing to 2 to 4 weeks of mindful tracking. This timeframe typically covers a full menstrual cycle and gives you a clear view of hormonal patterns, emotional rhythms, and the effects of lifestyle changes.
What to Track
Use a journal, a printable tracker, or a digital tool to log daily or weekly reflections on the following:
🌟 Wins and Resets
Celebrate the small things: a nourishing breakfast, a midday walk, saying no without guilt, or getting to bed on time. These micro-wins are signs of resilience building.
🌙 Sleep Quality
How long did you sleep? Was it restful? Did you wake feeling refreshed or groggy? Note any nighttime waking patterns or trouble falling asleep.
⚡ Energy Levels
Rate your energy on a scale of 1–10 throughout the day. Do you feel energized in the morning? Experience a midafternoon crash? Wired at night?
🌸 Cycle Phase (If Applicable)
Track your menstrual cycle days and note where ovulation likely occurred. Pay attention to PMS, spotting, heavy bleeding, or irregular timing—these are key hormonal clues.
😖 Notable Symptoms
Record physical or emotional changes such as anxiety, bloating, cravings, breast tenderness, mood swings, acne, or brain fog. Don’t forget digestive issues—they’re often tied to hormonal shifts.
🔄 Stress Triggers
What events, thoughts, or situations raised your stress levels today? Examples might include work pressure, family conflict, poor sleep, skipped meals, or emotional overwhelm.
Why It Matters
Tracking helps you:
- Connect symptoms to cycle phases and stress exposure
- Recognize what lifestyle changes are making a difference
- Identify trends (e.g., “I always feel more anxious in the luteal phase” or “Skipping meals makes me crash”)
- Prepare for conversations with your healthcare provider
- Stay engaged without obsessing
It’s not about being perfect—it’s about becoming informed. Over time, you’ll start to anticipate your body’s needs instead of reacting to discomfort.
Final Words
The relationship between cortisol and progesterone is a reflection of how your body prioritizes survival over balance. When stress becomes the norm, your system wisely redirects resources toward making cortisol—often at the expense of calming, cycle-regulating progesterone.
But this doesn’t mean your hormones are broken. It means they’re responding exactly as they should to the signals they’re receiving.
By supporting your body with rhythm-friendly routines, nourishing foods, and stress-reducing practices, you can rebuild hormone resilience. You don’t have to live with anxiety, poor sleep, irregular cycles, or burnout as your baseline.
You deserve to feel steady, supported, and hormonally strong—at any age.
