Cortisol and menopause are two powerful forces that shape a woman’s experience in midlife, often in ways that feel overwhelming or confusing. As women transition through menopause, hormonal shifts affect not only estrogen and progesterone but also the body’s stress hormone, cortisol. While cortisol plays a crucial role in managing stress, energy, and inflammation, imbalances during menopause can intensify symptoms like weight gain, sleep disturbances, and mood swings.
In this article, we’ll explore how cortisol and menopause interact, why stress becomes harder to manage after 40, and — most importantly — what steps you can take to restore balance and feel better.
What Is Cortisol?
Cortisol is a vital hormone produced by the adrenal glands, located just above your kidneys. Often referred to as the “stress hormone,” cortisol plays a central role in your body’s response to physical, emotional, and environmental stressors. However, cortisol does much more than manage stress — it also helps regulate blood sugar, control inflammation, influence metabolism, and maintain energy levels throughout the day.
Under healthy conditions, cortisol follows a natural daily rhythm. It rises sharply in the early morning to help you wake up feeling alert and energetic, then gradually declines throughout the day, reaching its lowest point at night to allow restful sleep. This daily cycle, known as the cortisol circadian rhythm, is essential for maintaining balance across many body systems.
When cortisol levels are properly regulated, they help you feel energized during the day, stay resilient under pressure, and recover easily from challenges. But when cortisol becomes chronically elevated or erratic — a common occurrence during midlife hormonal changes — it can disrupt sleep, increase cravings, promote weight gain, and strain the body’s ability to recover from stress.
How Menopause Affects Cortisol Levels
During the menopausal transition, your body undergoes a significant hormonal shift — and cortisol doesn’t stay untouched. The connection between cortisol and menopause becomes particularly important as levels of estrogen and progesterone decline.
Progesterone, often referred to as the body’s natural calming hormone, begins to drop in perimenopause. This hormone has a soothing effect on the nervous system, helping to keep cortisol in check. As progesterone wanes, many women notice they feel more anxious, reactive, or overwhelmed — a sign that cortisol may be becoming dysregulated.
Estrogen also plays a role in buffering the effects of cortisol. As estrogen declines, the body may become more sensitive to stress, leading to stronger cortisol surges in response to everyday events. This heightened reactivity can feel like you’re always “on edge,” even when nothing major is going on.
To make things more complicated, sleep disturbances — a hallmark of menopause — further disrupt the cortisol rhythm. When you don’t sleep well, your body produces more cortisol the next day, which then makes it harder to fall asleep the following night, creating a vicious cycle.
The hormonal upheaval of menopause doesn’t just cause hot flashes and irregular periods — it alters how your body handles stress, metabolizes energy, and maintains emotional balance, with cortisol at the center of it all.
Signs of Cortisol Imbalance During Menopause
You feel exhausted during the day but have a second wind at night — a classic sign of disrupted cortisol rhythm.
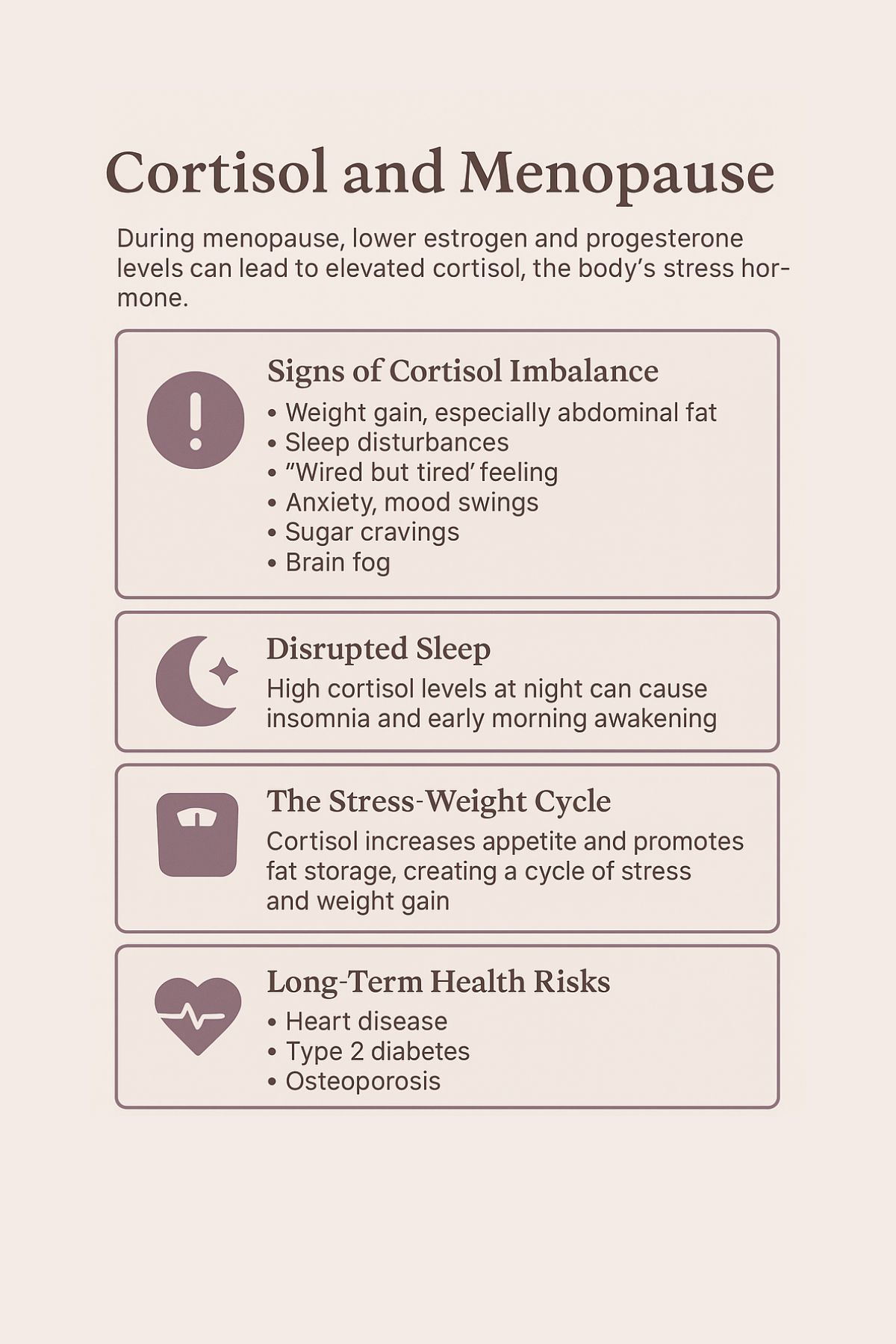
😴 Poor Sleep Quality
Trouble falling asleep or waking up between 2–4 a.m. (when cortisol naturally rises) may point to adrenal dysregulation.
⚖️ Stubborn Weight Gain, Especially Around the Belly
High cortisol promotes fat storage in the abdominal area — even without overeating — and makes it harder to lose weight.
🍬 Cravings for Sugar, Salt, or Carbs
Cortisol impacts blood sugar stability, leading to rollercoaster-like cravings and energy crashes.
😡 Mood Swings, Anxiety, or Irritability
Reduced progesterone and increased cortisol make the nervous system more reactive. You may feel more overwhelmed by situations you used to handle with ease.
🧠 Brain Fog and Forgetfulness
Chronic stress from elevated cortisol can interfere with memory, focus, and mental clarity.
💓 Increased Heart Rate or Blood Pressure
Persistent stress can keep your body in a “fight-or-flight” state, even when you’re resting.
Many of these symptoms overlap with menopause itself, which can make it hard to identify cortisol as the underlying driver. But recognizing these signs is the first step toward restoring hormonal harmony — and your quality of life.
The Vicious Cycle: Cortisol, Sleep, and Weight Gain
The relationship between cortisol and menopause creates a domino effect that can trap women in a frustrating cycle of poor sleep, low energy, and weight gain — especially around the midsection.
💤 Cortisol Disrupts Sleep
Under normal conditions, cortisol should be low at night to allow melatonin — your sleep hormone — to rise. But during menopause, when stress is poorly regulated, cortisol may spike in the evening or early morning hours. This makes it harder to fall asleep or leads to early waking, often around 3 a.m., with a racing mind and a restless body.
🍳 Poor Sleep Elevates Cortisol
After a bad night’s sleep, your body compensates by producing more cortisol the next day. This elevated cortisol increases appetite, especially for high-sugar, high-fat foods, and reduces your ability to regulate blood sugar effectively.
⚖️ High Cortisol Promotes Belly Fat
Cortisol doesn’t just increase hunger — it also changes how your body stores fat. Chronically high cortisol encourages fat storage around the abdomen. This visceral fat is metabolically active and linked to higher risks of insulin resistance, heart disease, and inflammation.
🔄 And the Cycle Repeats
The more belly fat you accumulate, the more inflammation your body produces. Inflammation can further disrupt sleep and stress regulation, leading to even more cortisol production — and so the cycle continues.
For women in menopause, this cortisol-sleep-weight loop can feel impossible to escape. But the good news is that small, consistent changes — like stress management, improved sleep hygiene, and balanced meals — can gradually help reset this hormonal cycle.
Long-Term Health Risks of Chronic High Cortisol After Menopause
When cortisol and menopause collide, it’s not just about short-term discomfort. Chronically elevated cortisol levels can have serious long-term health implications, particularly for women navigating life after 40.
❤️ Increased Risk of Cardiovascular Disease
High cortisol contributes to elevated blood pressure, cholesterol imbalances, and inflammation — all key risk factors for heart disease. With estrogen levels declining during menopause (which once offered some cardiovascular protection), the impact of cortisol becomes even more pronounced.
🍬 Blood Sugar Imbalances and Type 2 Diabetes
Cortisol raises blood glucose levels to prepare your body for “fight or flight.” But when this response becomes chronic, it leads to insulin resistance, making it harder to maintain healthy blood sugar and increasing the risk of developing type 2 diabetes.
🦴 Bone Loss and Osteoporosis
Cortisol can interfere with bone-building cells and calcium absorption. Combined with lower estrogen, this creates a double hit to bone density, increasing the risk of fractures in postmenopausal women.
🧠 Cognitive Decline and Memory Issues
High cortisol over time can shrink the hippocampus — the part of the brain responsible for memory and learning. Many women in midlife report “brain fog,” forgetfulness, or mental fatigue, which may be linked to stress hormone overload.
🌿 Weakened Immune Function and Chronic Inflammation
Cortisol suppresses immune activity in the short term, but chronic stress can leave the body inflamed and vulnerable to illness, autoimmune flares, and slower recovery from infections.
Understanding these risks helps shift the narrative from “this is just menopause” to “this is my body asking for support.” Addressing cortisol imbalance is not only about feeling better now — it’s a preventive step toward aging well and staying vibrant in the decades to come.
How to Support Healthy Cortisol Levels During Menopause
Supporting the balance between cortisol and menopause doesn’t require drastic measures — small, consistent lifestyle shifts can make a powerful difference. By focusing on restoring your body’s natural rhythms and building resilience to stress, you can ease many of the symptoms linked to cortisol imbalance.

🧘♀️ Stress Management Techniques
- Deep Breathing and Meditation: Just a few minutes of deep, slow breathing or mindfulness each day can lower cortisol levels. Apps and guided meditations can help you get started.
- Gentle Movement: Yoga, stretching, and tai chi help lower stress hormones without overtaxing the body.
- Nature Time: Being in nature (even a short daily walk outside) helps regulate cortisol and promotes emotional calm.
😴 Prioritize High-Quality Sleep
- Create a Sleep Ritual: Consistent bedtime routines — like dimming lights, limiting screens, and practicing relaxation exercises — signal your body it’s time to wind down.
- Protect Your Sleep Window: Aim for 7–9 hours of sleep per night. Keep your bedroom cool, dark, and quiet to promote deeper rest.
- Limit Late-Night Stimulants: Caffeine, alcohol, and heavy meals close to bedtime can spike cortisol and disrupt sleep.
🍽️ Balance Blood Sugar
- Eat Regular, Balanced Meals: Focus on meals with protein, healthy fats, and fiber to stabilize blood sugar and minimize cortisol spikes.
- Avoid Extreme Dieting: Skipping meals or extreme calorie restriction stresses the body and elevates cortisol.
🏋️ Exercise Smart, Not Harder
- Strength Training and Moderate Cardio: Build strength and cardiovascular health without overexerting your adrenal system.
- Listen to Your Body: If you feel more drained than energized after workouts, it’s a sign to scale back.
🌿 Nutritional Support for Adrenal Health
- Magnesium: Found in leafy greens, nuts, and seeds, magnesium helps regulate cortisol and promote relaxation.
- B Vitamins: Crucial for energy metabolism and adrenal support. Sources include whole grains, eggs, and legumes.
- Adaptogens (with Professional Guidance): Herbs like ashwagandha, rhodiola, and holy basil may help regulate stress responses, but it’s best to consult your healthcare provider before starting supplements.
By consistently layering in these small habits, women can strengthen their stress resilience and create a more stable, energized, and balanced experience of menopause — one where cortisol works for you, not against you.
Cortisol and Menopause: When to Seek Help
While many women can improve the balance between cortisol and menopause with simple lifestyle changes, there are times when professional help is necessary. Ignoring persistent symptoms can lead to worsening health issues over time, so it’s important to recognize when to seek support.
🚩 Warning Signs That Need Attention
- Severe or persistent fatigue that doesn’t improve with rest
- Chronic insomnia despite good sleep habits
- Significant mood changes like depression, anxiety, or irritability
- Unexplained weight gain, particularly around the abdomen
- Frequent infections, slow wound healing, or signs of a weakened immune system
- Irregular or very high blood pressure readings
These symptoms may indicate deeper adrenal dysfunction or other hormonal imbalances that require targeted interventions.
Conculsion
The interplay between cortisol and menopause is a critical but often overlooked piece of the midlife health puzzle. As estrogen and progesterone decline, cortisol can become harder to regulate, leading to a cascade of symptoms like weight gain, sleep disturbances, mood swings, and low energy. Left unchecked, chronic cortisol imbalance can also increase long-term risks for heart disease, diabetes, osteoporosis, and cognitive decline.
The good news is that you’re not powerless. Small, intentional lifestyle changes — from managing stress and supporting sleep to balancing blood sugar and gentle movement — can go a long way in restoring cortisol harmony. And if symptoms persist, expert guidance from your healthcare team can offer deeper insights and more targeted solutions.
You deserve to thrive, not just survive, through menopause. By understanding and supporting your body’s evolving needs, you can break the stress-weight cycle, reclaim your energy, and step into the next chapter of life feeling stronger, clearer, and more resilient than ever.
